The Vast Overtreatment of Blood Pressure
First, they did it with cholesterol and statins. Now, they're doing it with 'high' blood pressure and medications, along with unrealistic (and unproven) salt restrictions.
STORY AT-A-GLANCE
High blood pressure (hypertension) is increasingly common, with more people diagnosed each decade
At least 25% of hypertension diagnoses are due to inaccurate measurements
The cause of hypertension is unknown for over 90% of patients
Aggressively treating blood pressure is believed to prevent cardiovascular disease but only has a limited effect on strokes, not heart disease
The correlation between high blood pressure and cardiovascular disease is often misinterpreted; impaired circulation causes blood pressure to rise, not the other way around
In this article, I discuss the limitations of conventional blood pressure perspectives and explore the actual causes of high blood pressure (hypertension)
Ever since I first encountered the medical field, something struck me as off about their relentless focus on blood pressure. Before long, I noticed that the blood pressures the same acquaintances (e.g., relatives, patients, friends) shared with me varied immensely. While pondering this, a talented practitioner and mentor once told me that the current medical paradigm fixates on blood pressure1 because it's easier to measure than blood perfusion (healthy blood flow).
Then, as I became more acquainted with the medical field, I began to notice a consistent pattern — whenever a drug existed that could treat a number or statistic, as the years went by, the acceptable number kept on being narrowed, making more and more people eligible to take the drugs that treated the number.
For example, as I discussed recently, once the statins drugs entered the market (which unlike their predecessors, could effectively lower cholesterol), the acceptable blood cholesterol levels kept on being lowered, and before long almost everyone was told they would die from a heart attack unless they started a statin — despite statins have an almost non-existing mortality benefit (e.g., taking them for five years at best makes you live 3 to 4 days longer2) and causing (often severe) side effects for roughly 20% of users.
In turn, since so many people have been severely harmed by the great statin scam, more and more people, such as comedian Jimmy Dore have begun to speak out against this:
Broadly recommending these drugs hence appears unconscionable, but as I showed in that article, these unjustifiable guidelines were a product of clever pharmaceutical marketing and targeted bribery of public officials. In today’s article, I will attempt to show how something similar happened with blood pressure management.
Conventional Blood Pressure Perspectives
Since blood vessels are elastic fluid filled structures, that fluid holds them under pressure. Blood pressure in turn, is typically measured by determining how much external force is needed to exceed the artery’s pressure and compress it so that blood no longer flows through it.
Low blood pressure (hypotension) is a problem because it prevents blood from reaching the areas where it’s needed, but in most cases, medicine instead focuses on the consequences of high blood pressure. Within the existing model, those consequences are:
Weakened blood vessels become more likely to break open and leak as higher blood pressure pushes against them. This for instance, is why Emergency Rooms aggressively lower the blood pressure of patients who show up with symptoms of "hypertensive emergency," such as a severe headache and a significantly elevated blood pressure.
Likewise, whenever a critical blood vessel ruptures (e.g., the aorta or one in the brain), once the bleed has been confirmed, the first step in managing it is to lower the patient’s blood pressure (so less blood leaks out) after which they are sent to surgery.
Excessive pressure on the arteries strains and damages them, causing the lining of the vessels to become damaged and gradually develop atherosclerosis.
Excessive blood pressure damages the internal organs (termed end-organ damage), leading to premature failure and early death (e.g., from a heart attack or kidney failure).
Because of this, high blood pressure is viewed as one of the greatest preventable causes of cardiovascular disease, and thus, ensuring a patient achieves sufficiently lowered blood pressure is a chief focus of all medical visits. Unfortunately, that chain of logic has quite a few holes in it.
Variable Blood Pressure
Blood pressure (BP) is highly variable, especially at the periphery, where it's typically measured. This variability — around 14 points3 — can lead to misdiagnosis of hypertension and unnecessary medication, which can lower BP too much, causing hypotension. One common form of this misdiagnosis is known as White Coat Hypertension, where the stress of visiting a doctor temporarily raises BP.
This affects 15% to 30%4 of patients diagnosed with hypertension. Guidelines recommend confirming hypertension with multiple measurements, including home monitoring, but this often doesn't happen.
Measurement errors, like using the wrong cuff size or not accounting for differing BP in each arm,5 contribute to the issue. It's estimated that 25% of hypertension diagnoses are incorrect.6 Moreover, there is often a poor correlation between peripheral BP (limbs) and central BP (inside the aorta).
Central BP, which is more closely linked to cardiovascular disease, can differ significantly from arm readings. Different BP medications also affect central and peripheral BP differently, adding complexity to treatment.
What Affects Blood Pressure?
If fluid at a set pressure tries to move through a tube, as the tube shrinks, the pressure it creates (e.g., on the walls of the tube) will increase, while if the tube enlarges, the pressure it exerts will decrease. The body continually controls where blood in the body goes by changing the heart rate and fully or partially constricting the arteries, allowing it to shunt blood to where it is most needed (e.g., by dilating arteries in that area).
Blood pressure is thus a product of two factors: the amount of blood in the arteries and the constriction or relaxation of the arteries containing it.
Note: Since arterial BP is greater than venous BP, it’s what’s measured externally (as veins compress long before arteries do, and only arterial blood has a signature pulsatile wave created by the heartbeat).
Since each heartbeat pushes blood into the arteries and hence increases the pressure within them, two different blood pressure values exist — the baseline pressure (known as the diastolic pressure or DBP) and the pressure when the heart contracts (known as systolic pressure or SBP). The blood pressure values you see (e.g., 140/90) represent the maximum and minimum.
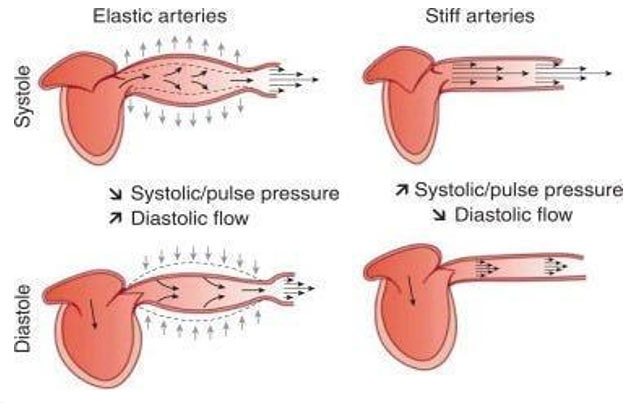
Note: One reason why this stretching is important is that when the vessels contract back to their normal size once the systolic pressure fades, that recoil pushes blood further along into the circulation.
Blood pressure lowering medications in turn work by some combination of:
Loosening the arterial walls
Reducing the total blood in circulation
Weakening the contraction of the heart
What Causes High Blood Pressure?
Most cases of high blood pressure (90% to 95% of them7) are what is known as "essential hypertension" or "primary hypertension" which is a fancy (and rarely questioned) way of saying "elevated blood pressure without a known cause." More importantly, the fact there is no known cause for most cases of elevated blood pressure has been a widespread belief in medicine for decades.
Typically, the only cause we hear about is "eating salt," despite the fact that the most detailed review of this subject8 found that drastic salt reduction typically results in less than a 1% reduction in blood pressure.
For the remaining 5% to 10% (known as secondary hypertension), recognized causes include reduced blood flow to the kidneys9 (which sets off a signal to raise the blood pressure because the kidney believes there isn’t enough blood perfusion), sleep apnea,10 or having a rare tumor11 that releases a blood pressure increasing hormone. Since the cause of most hypertension is unclear, medicine focuses on risk factors like age, diabetes, salt intake, obesity, stress, and family history.
Note: Effectively addressing anxiety can often cure a high blood pressure that would otherwise be perpetually medicated.
Atherosclerosis and Blood Pressure
Many of my colleagues became suspicious of the traditional blood pressure model after noticing that circulatory impairments often occurred alongside rising blood pressure, not as a result of long-term damage from it.
This led us to conclude that elevated blood pressure might be a compensatory response to inadequate blood flow, similar to how the kidneys raise blood pressure when they don’t receive enough blood. Several factors support this idea:
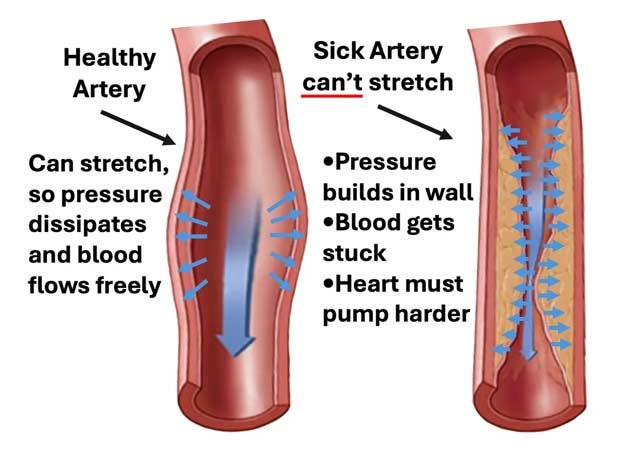
Arterial stiffening — Calcified arteries can't expand as effectively, raising blood pressure as they become less able to release pressure.
Measurement inaccuracy — Blood pressure cuffs may overestimate pressure in stiffened arteries, especially in those with severe atherosclerosis,12 leading to higher readings than the actual pressure (as the hardened arteries require more pressure to compress).
Endothelial dysfunction — The blood vessel lining releases nitric oxide to dilate vessels and decrease pressure. When this function fails,13 it precedes atherosclerosis and increases blood pressure, suggesting the problem is with endothelial health, not high blood pressure itself.
Sympathetic reflex — When the body rapidly loses a significant amount of blood,14 a reflex triggers increased heart rate and vessel constriction to raise blood pressure, a common response in critical conditions.
This all suggests that high blood pressure may be more of a symptom than the root cause of circulatory issues.
Zeta Potential and Blood Pressure
Zeta potential, a crucial component of health, quantifies the electrical charge difference between colloidal particles in a liquid. When sufficient zeta potential is present, those particles stay separated, while in disease states, they clump together. Many dangerous agents (e.g., aluminum, the spike protein, and the dangerous microbes) disrupt zeta potential, which commonly leads to blood cells in the body clumping together and microstrokes.
This process is recognized by many medical systems (e.g., Chinese medicine has the diagnosis blood stasis,15 which is almost identical to blood sludging,16 a concept many Western researchers previously demonstrated was a root cause of disease) and with appropriate examination can easily be detected (e.g., there are many neurological deficits frequently triggered by microstrokes which can be detected with the appropriate examination). Sludged blood, in turn, can raise blood pressure by:
Create a backlog in the circulation, which would increase the pressure on it (since blood would push against the arterial walls instead of being pushed forward).
Signal the body to increase its blood pressure so the pockets of sludged blood could be pushed along.
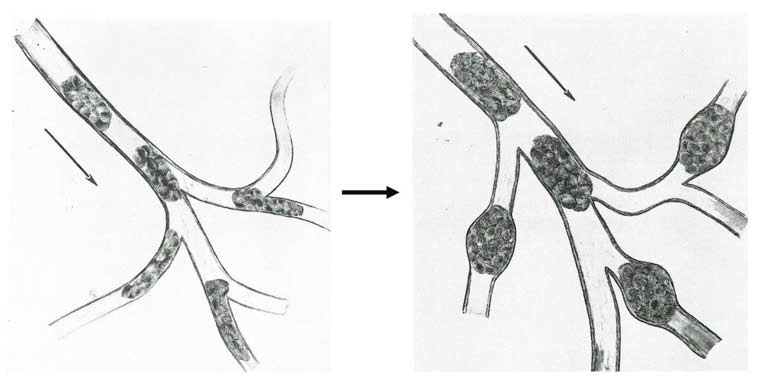
Directly stretch the smaller blood vessels, thereby increasing their pressure (and simultaneously "stiffen" the arteries because the clumps of sludge would have significantly more resistance to compression than dispersed blood cells).
To illustrate: The blood sludging researchers17 repeatedly observed small arteries (e.g., those in the eyes) become stretched by larger sludges.
Additionally, they observed that once the pockets of sludge formed, the pressure build-up caused plasma (the non-cellular component of the blood) to begin leaking out into the tissues, leading to things like edema (swelling). Thus, the remaining blood became even more concentrated in these sludge pockets.
Note: Once the zeta potential concept was applied to this phenomenon, it was noted18 that like other colloids, if their motion was slowed, blood cells would clump together and existing clumps would enlarge. This may in part explain why immobility and a lack of exercise are so detrimental to cardiovascular health.
While blood sludging primarily affects smaller vessels, causing microstroke-like injuries, it also impacts larger vessels by obstructing the vasa vasorum,19 the small blood vessels that nourish arteries. When the blood supply to the vasa vasorum is cut off, the endothelial lining of its artery dies,20 leading to high blood pressure and cardiovascular disease.
Note: Motion breaks up these clumps, which may partly explain why immobility is linked to heart disease.21
In turn, zeta potential researchers believed poor zeta potential was linked to atherosclerosis and found restoring zeta potential to be one of the most effective ways to normalize blood pressure (and treat heart disease).
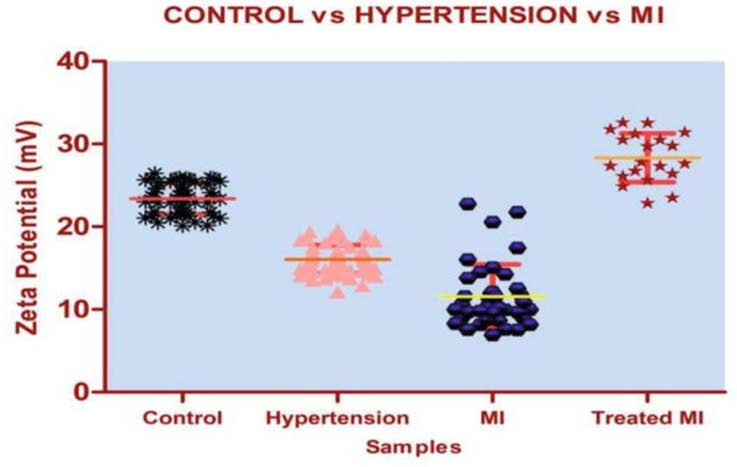
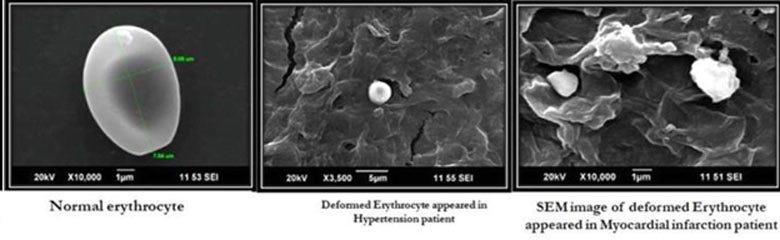
A 2019 study22 supports this. It compared the zeta potential of 64 patients with hypertension to 50 controls. It found the controls had an average zeta potential of -23.39 mV, while hypertensive patients had a zeta potential of -16.06 mV, and that heart attack (MI) patients had even worse zeta potentials.
Note: -10mv to -15mv is the threshold at which blood cells typically begin to agglomerate, while -16 to -30mv is the delicate dispersion at which cells can rapidly clot when needed (e.g., due to an arterial injury).
Likewise, when their blood was looked at, there was significantly greater clumping:
Note: The Chinese Medicine equivalent of this process (termed blood stasis) is also correlated with high blood pressure.
Does High Blood Pressure Cause Heart Disease?
High blood pressure is often associated with heart disease and serious vascular issues like strokes and organ damage when blood pressure spikes (e.g., SBP over 200). However, there is little evidence that small increases in blood pressure cause problems.
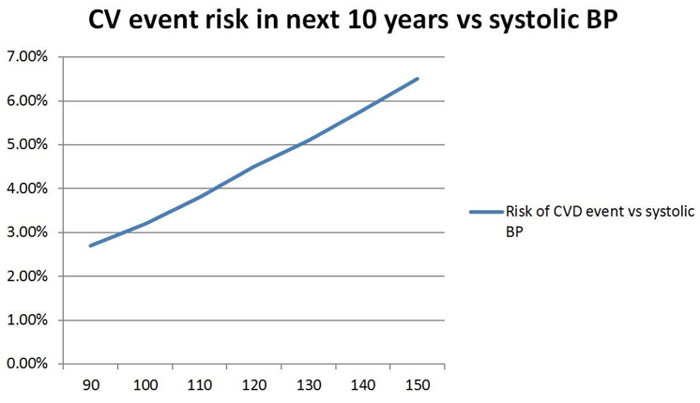
This belief stems largely from the Framingham study,23 which suggested a linear relationship between blood pressure and the risk of death — implying that continually lowering blood pressure reduces mortality.
That has been the basis for many things, like continual recommendations for lower and lower blood pressures or the highly erroneous cardiovascular disease risk calculator everyone uses to justify prescriptions (but was found to overestimate one’s risk of dying by 600%24). For example, this is what the calculator shows25 for an otherwise healthy male when only their blood pressure is adjusted.
In turn, there are a few major issues with this paradigm:
No optimal BP — A SBP below 90 is known to be dangerous, yet the model suggests continually lowering it. The NIH admitted this.26
Biological relationships are rarely linear.
Lack of evidence — There's no actual proof27 that lowering blood pressure from, say, 100 to 90 provides any benefit.
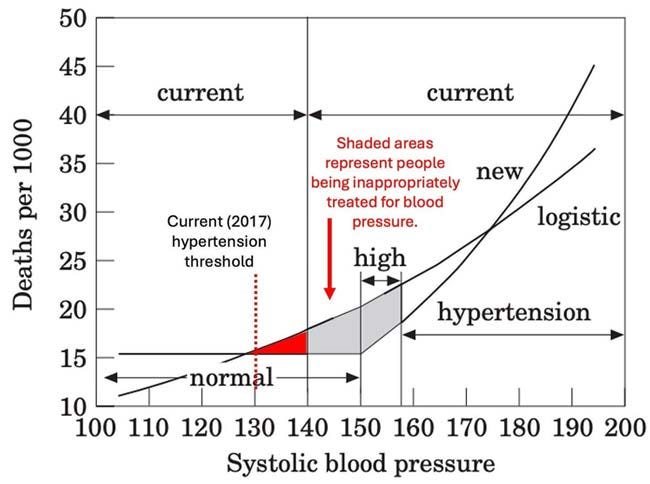
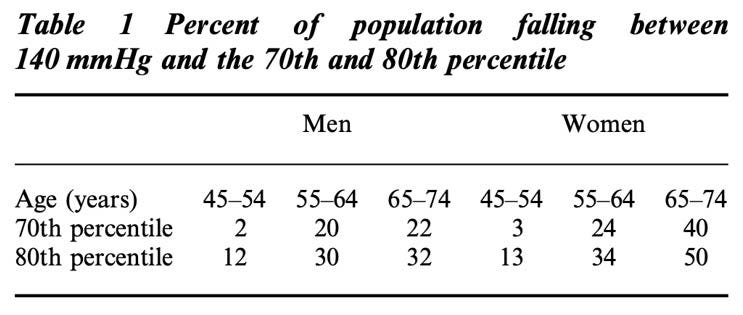
Flawed data — A re-analysis of the Framingham data in 2000 showed that blood pressure’s impact on mortality isn't linear.28 Instead, the risk only rises exponentially after a threshold is passed, typically when blood pressure exceeds 70% to 80% of what’s normal for age and gender.
Note: When this (forgotten) paper was published,29 the conventional blood pressure thresholds were less aggressive. I modified its graph to match the current guidelines.
After the paper was published, it was mostly ignored but eventually received this response30 (which again illustrates how resistant medical dogmas are to evidence that refutes them):
"The National Institutes of Health’s National Heart, Lung, and Blood Institute (NHLBI) issued a statement regarding Port’s findings saying that they found it 'thought provoking' but 'After careful review of this study, the NHLBI finds that it does not offer a basis for changing the current hypertension guidelines.'"
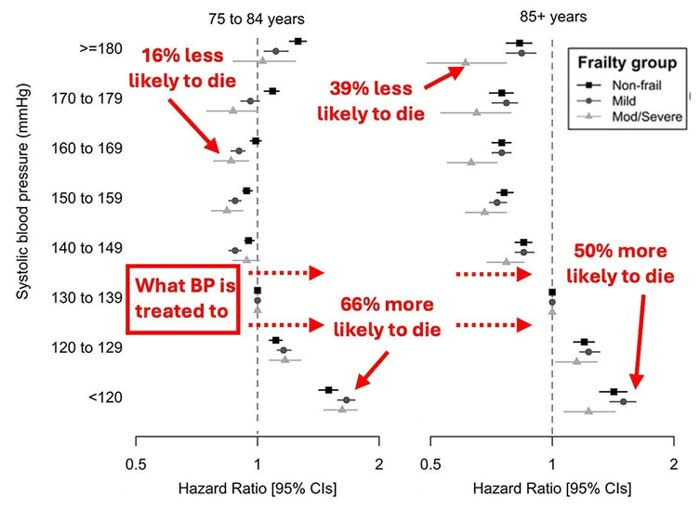
Likewise, consider a study31 of 415,980 patients obtained through their electronic health records which again shows that threshold and demonstrates that medicine treat blood pressure to a dangerously low level:
Note: In addition to a SBP below 130 significantly increasing the chance of death, this study also found a diastolic blood pressure (DBP) below 80 (a common consequence of blood pressure lowering medications) made patients 8% to 19% more likely to die.
Furthermore, another smaller study32 of 800 adults over 60 found a DBP under 80 made participants 90% to 190% more likely to die and that a SBP under 120 was associated with a higher risk of death.
Finally, since slightly elevated blood pressures are far more common than highly elevated ones, each time the treatment target is lowered by a small amount, a large number of people get pushed onto these drugs, especially the elderly (as their blood pressure rises to compensate for the decreased health of their arterial system).
Because of this, a large number of people are diagnosed as having dangerous hypertension in the linear model but not in the more accurate threshold model.
Sadder still, these numbers are even vastly worse when 130 is set as the threshold instead of 140 (which is what happened in 2017). For example, 77% of adults over 64 meet this threshold, and 79% of those over 74 do.
Blood Pressure Mortality Studies
Despite widespread belief, there's little evidence that lowering moderately elevated blood pressure improves survival. In fact, major studies have shown minimal benefits.
In 1973, a large UK study involving 17,354 patients33 with moderately high blood pressure (averaging 158/98 in men and 166/99 in women) compared beta blockers, diuretics, and placebos was conducted to prove lowering blood pressure stopped heart attacks. It found no significant difference in coronary event rates or death rates between groups.
The only notable benefit was a slight reduction in (likely hemorrhagic) strokes, but side effects were common, causing 25% of participants to drop out.
After this trial, the term "heart disease" was rebranded as "cardiovascular disease," creating the illusion that blood pressure treatment prevented heart attacks when the actual benefit was a small reduction in strokes.
A 2009 Cochrane34 review, and later a 2020 review,35 also found little benefit from lowering systolic blood pressure (SBP) below 135 compared to 140. In fact, the harms, including kidney damage, often outweighed the benefits.
Conclusion
The rush to market blood pressure-lowering drugs began with minimal proof of long-term benefit, based on a few short-term studies for very high blood pressure. Over time, without solid evidence, the threshold for treatment has been continuously lowered, leading to more people, particularly the elderly, being prescribed these drugs. Around 60 million36 Americans (23%) now take them, despite the elderly being more vulnerable to low blood pressure due to calcified arteries.
In turn, every awake physician I know gradually reached the conclusion that the current hypertension paradigm was flawed and hence became much more conservative when they would directly treat blood pressure while simultaneously having a large focus on reversing the causes of high blood pressure rather than trying to treat it with medications. It is thus my sincere hope we can bring public awareness to the dangers of over treating blood pressure.
Author's note: This is an abridged version of a longer article about the great blood pressure scam which goes into greater detail on the points mentioned here, the dangers of blood pressure medications and natural ways to safely lower blood pressure. That article and its additional references can be read here.
A Note from Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician from the Midwest and a longtime reader of Mercola.com. I appreciate AMD's exceptional insight on a wide range of topics and am grateful to share it. I also respect AMD’s desire to remain anonymous since AMD is still on the front lines treating patients. To find more of AMD's work, be sure to check out The Forgotten Side of Medicine on Substack.
Disclaimer: The entire contents of this website are based upon the opinions of Dr. Mercola, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked.
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Mercola and his community. Dr. Mercola encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. The subscription fee being requested is for access to the articles and information posted on this site, and is not being paid for any individual medical advice.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.