Popular Drug Causes ‘Prescribing Cascades’ That Lead to Poor Health
What looks like a new medical problem may actually be a drug reaction - and when that connection is missed, patients can be pulled into a cycle that adds medications instead of removing the cause.
STORY AT-A-GLANCE
The prescription drug gabapentin is now heavily prescribed to millions, despite limited approved uses and a growing link to drug-driven cascades like edema, which leads to unnecessary diuretics
Aggressive off-label promotion pushed gabapentin into mainstream use, leading to millions of seniors taking it for unapproved conditions and increasing the risk of edema being misdiagnosed as a new disease instead of being a side effect
Doctors often misinterpret gabapentin-induced swelling, triggering extensive testing, added prescriptions, fragmented care, and harmful complications such as electrolyte imbalances and falls
Certain groups face higher risk of prescribing cascades, especially adults in their 60s and 70s and anyone already taking multiple medications from different prescribers
Rising prescription spending signals a need to reassess medication lists, recognize signs of overmedication, and take proactive steps to reduce unnecessary drugs and protect long-term health
Polypharmacy is a growing health problem in America, particularly among the elderly. According to Johns Hopkins Medicine, around one-third of American adults in their 60s and 70s are taking five or more prescription medications every day for various conditions, such as depression, arthritis, and high blood pressure.1
That’s because the initial drug usually causes side effects, and to treat those, new drugs are prescribed. Within this context, a well-known drug is often left out in the conversation — gabapentin.
According to The New York Times, about 5.7 million older adults have taken gabapentin, and most were not for the conditions it was originally approved to treat. The U.S. Food and Drug Administration approved gabapentin in 1993 for epileptic seizures and, in 2002, for postherpetic neuralgia.2 Yet today, it’s commonly prescribed for a wide range of off-label uses, including alcohol dependence and sciatica.
So why the surge in gabapentin use? Much of it traces back to aggressive marketing. Warner-Lambert, the drug’s original manufacturer, promoted gabapentin for unapproved uses to boost sales — tactics that eventually led to a $430 million settlement for illegal marketing. By the time penalties were handed down, the drug’s widespread off-label use was already firmly in place.
Experts are now linking its widespread use to an increased risk for a “prescribing cascade.”3 This is a situation wherein a prescription drug causes an adverse event, which becomes mistaken as a new condition. This causes the doctor to prescribe a new medication, hence the cascade.4 Within the context of gabapentin, it causes edema, and patients are subsequently prescribed loop diuretics arbitrarily, making the situation worse.5
Gabapentin Is a Frequent Trigger of Prescribing Cascades
In a study published in JAMA Network Open, researchers investigated how often gabapentinoids spark a prescribing cascade in older adults. For the analysis, they manually reviewed medical charts to understand exactly what clinicians thought, documented, ordered, and prescribed. Their goal was to determine how often the swelling was recognized as a gabapentin side effect and how often it was mistaken for a brand-new disease.6
Framework of the study — A total of 120 U.S. veterans who had recently been prescribed a gabapentinoid and then received a loop diuretic within six months were selected for the study. These were not people diagnosed with heart failure or kidney disease before the swelling. They were adults seeking to address their nerve pain or similar symptoms, and the swelling emerged only after the gabapentinoid entered the picture.
According to researchers, clinicians rarely mention the drug as a cause of the edema, even though gabapentin is known to produce fluid buildup.7 That omission sets the stage for every problem that follows and explains why so many older adults find themselves on a diuretic loop despite having no underlying cardiac or renal condition.
Doctors were consistently mistaken — Details from the chart reviews reveal how consistently doctors attributed the swelling to heart failure or venous disease rather than the gabapentinoid itself. The authors noted that “clinicians almost never explicitly considered gabapentinoid adverse drug effects in their management of edema,” which means your doctor might think your swollen legs reflect a new disease instead of a drug reaction.
Once that incorrect assumption enters your health records, it becomes extremely hard to undo. Every specialist who reads your medical history assumes the new disease is real, not medication-induced. This leads to repeat testing and more appointments that drain your time, money, and energy.
The implications of overprescription — Several patients went through what the researchers described as a “care cascade,” which included echocardiography, ultrasound tests, and multiple follow-up visits before the loop diuretic was added. Each of those tests is designed to search for heart or vascular conditions — problems that are not truly there.
It’s easy to assume that extra testing keeps you safe, but in this study, it did the opposite. It delayed the correct remedy (removal of the drug causing the problem) and increased the odds of ending up on a powerful diuretic that forces kidneys to work harder.
Drugs are prescribed haphazardly — In roughly two-thirds of cases, the clinician who prescribed the gabapentinoid was not the same clinician who prescribed the diuretic. This kind of fragmented care makes it extremely hard to connect the dots.
You know your full medication story, but the doctor who examines you for swelling might not. When they don’t know what the original doctor prescribed or why, it becomes far easier for them to treat the symptom rather than address the cause, setting the stage for polypharmacy.
How far the cascade reached — Downstream problems after the diuretic included electrolyte abnormalities and falls, two issues that can significantly endanger your health.
When a diuretic pulls too many electrolytes out of your system, your blood pressure drops, dizziness increases, and your balance suffers. That combination sends many older adults to the emergency room. The study showed that these complications were not random — they followed the exact moment the diuretic was added to treat the swelling caused by the gabapentinoid.
The study also sheds light on rates of misattribution — Only a very small percentage of clinicians recognized gabapentin as the source of the edema and adjusted or discontinued the medication accordingly.
The cascade often unfolded gradually — Swelling appeared weeks after the gabapentinoid started, and the diuretic prescription followed only after multiple tests and evaluations failed to find another explanation. That slow timeline makes it more difficult to attribute the effect to the proper cause, i.e., the medication. When symptoms do not appear immediately after the start of a new drug, clinicians often dismiss a medication link.
Differences between participant groups — Patients with more fragmented care had a higher likelihood of entering the prescribing cascade.
So, if you see multiple specialists, or if different clinicians manage your pain versus your general health, consolidation becomes very important. Every new prescriber adds distance between your medication list and the person making decisions about your symptoms. It becomes easier for them to misread the situation and harder for them to notice that a drug is causing the new symptom.
Older Adults Face a Much Higher Risk for Prescribing Cascade
In a related study published in the Journal of the American Geriatrics Society, researchers set out to discover who is most likely to experience the gabapentinoid prescribing cascade. Instead of looking only at a small group of individuals (like the previous study), this particular analysis cast a wider net, using national prescription data to track the sequence of medication starts across a very large population.8
The goal was to see whether loop diuretics were consistently prescribed after gabapentinoids and to determine which personal or clinical factors increased that likelihood.
Prescribing cascades are widespread — The study involved 151,442 people who received gabapentinoids for pain or related conditions. They were community-dwelling older adults who were living independently or semi-independently, dealing with chronic pain, and age-related medical issues. Of those, 1,599 people developed a prescribing cascade.
Older patients are commonly affected — Seniors in their late 60s and early 70s experienced the prescribing cascade more often than those aged 85 years old and older. At first glance, that may seem odd, but clinicians tend to be more cautious when prescribing for people in advanced ages, and they’re more flexible when it comes to reducing the number of prescriptions, too.
The number of medications you take affects your risk of the cascade — According to the researchers, older adults who were already taking 10 or more medications had significantly higher odds of receiving a loop diuretic after a gabapentinoid. Even those taking five to nine medications faced increased risk compared to individuals on four or fewer.
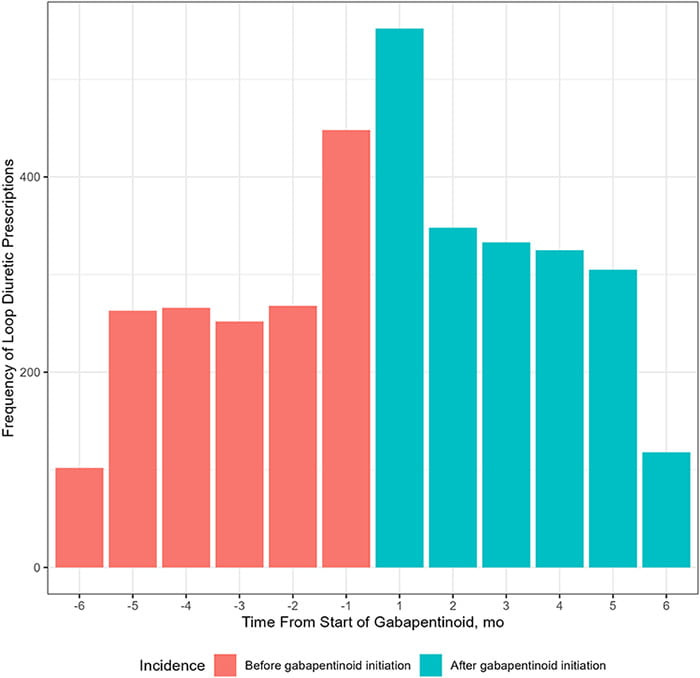
The study also looked at how medication timing influenced the cascade — The researchers used a method that compares whether loop diuretics appeared more often after a gabapentinoid than before, and the results were clear — there was a consistent timeline in which gabapentinoids come first, swelling comes next, and loop diuretics follow.
Anyone can be affected by a prescribing cascade — Beyond age and medication count, no single factor sharply defined who was at risk. The researchers found broad vulnerability across the entire older adult population.
The prescribing environment itself influences your risk — Similar to the previous study, this one also highlighted the impact of fragmented care in influencing the risk of creating a cascade.
If one clinician prescribes your gabapentinoid and a different clinician evaluates your swelling, neither may connect the dots. This lack of continuity increases your chance of receiving a loop diuretic instead of having the original drug adjusted or removed.
Are You Taking Too Many Prescription Drugs?
Based on data compiled by the Peter G. Peterson Foundation, Americans are spending more money on prescription medication compared to other nationalities.9 It’s estimated that Americans spend around $1,400 for prescriptions per year. Second are the Germans with $1,000, and third are Canadians with $865.10
Do you really need all the meds you’re taking? It’s good practice to sit down with your prescribing doctors on a regular basis to review all the medications you’re taking and assess their usefulness and whether any of them might be causing side effects. Here are some common factors that put you at risk for a prescribing cascade:11
You visit multiple doctors — You may think that all the different specialists you visit communicate with each other and exchange notes on how to help you address your health concerns. However, that rarely happens.
If you see one specialist for a particular issue and another specialist for a different problem, they oftentimes do not know what the other doctor has prescribed, or exactly why. It’s important to review your medical records at each specialist and update the records at each doctor’s office when you add or delete a prescription.
New health conditions appear — If you’ve been taking several medications, new health conditions and symptoms may appear due to interactions. Before taking a new prescription from your doctor, always do your due diligence and ask for possible interactions and side effects. Record the dates of symptom onset and review them with your prescriber.
You belong to a high-risk group — If you’re over the age of 65, you are more likely to be overprescribed medications. According to the Canadian Deprescribing Network, women are also at higher risk because they have a longer life expectancy, and their physiology increases the risk of adverse drug events.12
You have access to good health care — Those with good health insurance may be at higher risk for polypharmacy. It’s not uncommon for people in this position to see multiple doctors who are unaware of the medications being prescribed.
You have trouble keeping up with your medication — When you’re taking too many prescription drugs, you may start having problems keeping up with the frequency and timing. This could signify that you’re on too many drugs, and a visit to your primary care physician is warranted.
Financial pressure — A potential sign that you might be taking more medication than is necessary is the added financial strain on your budget.
Strategies to Help Reduce Your Dependency on Medications
While some drugs may be essential, others might no longer serve a purpose — or were never needed in the first place. Reducing unnecessary medications can help you cut costs and lower your risk of side effects or harmful drug interactions. Here’s how to get started:
List all medications you’re currently taking — Write down every prescription and over-the-counter product (OTC) you’re using. Bring that list to your primary care doctor and review anything prescribed by other specialists and ask which ones are truly needed and which ones can be replaced with healthy lifestyle changes.13
It would be wise to repeat this strategy once a year and again after any hospital stay, since it’s common to be sent home with medications that were meant only for short-term use.
Create a simple chart that includes the drug name, the reason you take it, the prescriber, the start date, and any side effects. This gives your primary care doctor a clear view of your situation in minutes. If you see multiple specialists, carry the chart to each appointment so every provider knows exactly what you’re taking, including OTC products.
Fill all prescriptions at one pharmacy — When a single pharmacist sees your full medication list, they can quickly identify dangerous interactions and give you reliable answers about OTC products and supplements.
Carefully pay attention every time someone prescribes new medications — Read the label carefully and spend time researching the drug yourself. If something concerns you, speak with your primary care doctor. They can help you find alternatives or a lifestyle plan that avoids adding yet another drug to your routine.
Frequently Asked Questions (FAQs) About Gabapentin-Related Prescribing Cascades
Q: Why is gabapentin a major concern in polypharmacy?
A: Gabapentin is widely prescribed to older adults despite limited FDA-approved uses. Its off-label promotion led millions to take it, increasing the risk of swelling, misdiagnosis, and prescribing cascades.
Q: What is a prescribing cascade and how does gabapentin trigger it?
A: A prescribing cascade occurs when a drug’s side effect is mistaken for a new illness, leading to another prescription. Gabapentin-induced swelling is often misread as heart or vascular disease, prompting unnecessary loop diuretics.
Q: How often do doctors overlook gabapentin-related side effects?
A: Studies show clinicians rarely recognize gabapentin as the source of edema. Most attribute symptoms to unrelated diseases, causing extra testing, more drugs, fragmented care, and higher health risks.
Q: Who is at highest risk for entering a gabapentin prescribing cascade?
A: Older adults in their 60s and 70s, individuals taking five or more medications, and those seeing multiple specialists face the greatest risk due to miscommunication and difficulty tracking medication effects.
Q: What steps help reduce the risk of polypharmacy and cascading prescriptions?
A: Keeping a detailed medication list, using one pharmacy, reviewing prescriptions regularly with a primary doctor, and questioning every new drug helps prevent unnecessary medications and harmful drug reactions.
Disclaimer: The entire contents of this website are based upon the opinions of Dr. Mercola, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked.
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Mercola and his community. Dr. Mercola encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. The subscription fee being requested is for access to the articles and information posted on this site, and is not being paid for any individual medical advice.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.




The issue of "prescribing cascades" due to drugs like gabapentin is a growing concern, especially for older adults who are already on multiple medications. When side effects like swelling are misdiagnosed as new conditions, additional drugs are prescribed, worsening the patient's health and leading to further complications. A proactive approach is needed to address this, such as regularly reviewing medications with healthcare providers, ensuring better communication between specialists, and reducing unnecessary prescriptions. By focusing on the root causes of symptoms and not just masking them with more medications, we can help break the cycle of overprescription and improve patient care.