Is Sunbathing More Important Than Vitamin D?
New research indicates that sunlight exposure produces another important hormone aside from vitamin D.
STORY AT-A-GLANCE
The vast majority, 95%, of the melatonin your body produces is made inside your mitochondria in response to near-infrared radiation from the sun. Only 5% of melatonin is produced in your pineal gland at night
During the day, near-infrared rays from the sun penetrate deep into your body and activate cytochrome c oxidase, which in turn stimulates the production of melatonin inside your mitochondria
Your mitochondria produce ATP, the energy currency of your body. A byproduct of this ATP production is reactive oxidative species (ROS), which are responsible for oxidative stress
Excessive amounts of ROS will damage the mitochondria, contributing to suboptimal health, inflammation and chronic health conditions such as diabetes, obesity and thrombosis (blood clots)
Melatonin mops up ROS that damage your mitochondria. Provided you get good sleep and plenty of sun exposure during the day, your mitochondria will be bathed in melatonin, thereby reducing oxidative stress
I have been absolutely fascinated with the association of sun exposure to health for nearly three decades. It was obvious to me that nearly all dermatologists are seriously confused about avoiding the sun, as sun exposure is essential to stay healthy.
I always knew there was some important fact we were missing, and I sincerely believe that in the MedCram video above, we learn what that is. Dr. Roger Seheult explains the ins and outs of how sunlight impacts your health — not only through increasing your vitamin D levels but through melatonin! It’s nearly two hours long, but well worth it if you have the time and are a fraction as fascinated by new science insights that could radically change your health as I am.
A condensed 25-minute version is included below. Seheult’s review is primarily based on the February 2020 paper,1 “Melatonin in Mitochondria: Mitigating Clear and Present Dangers,” published in the Physiology journal. It’s written by the best researcher in melatonin, Russel Reiter, Ph.D., whom I first heard lecture on melatonin over 25 years ago. This paper is one of the best papers I’ve read in a long while and you can access the full paper for free.
Melatonin Is Produced in Response to Sun Exposure
To summarize the key finding before we dive into the nitty-gritty, the vast majority of the melatonin your body produces — 95% — is actually made inside your mitochondria in response to near-infrared radiation from the sun. Only 5% of melatonin is produced in your pineal gland.
It is important to note that melatonin supplements, contrary to what you might expect, do not wind up in your mitochondria where they are needed most to quench the damage from oxidative stress produced in the electron transport chain.
Melatonin, of course, is a master hormone,2 a potent antioxidant3 and antioxidant recycler,4 and a master regulator of inflammation and cell death.5 These functions are part of what makes melatonin such an important anticancer molecule.6
Melatonin has also been shown to be an important part of COVID treatment, reducing incidence of thrombosis and sepsis7 and lowering mortality.8 9 As noted by Seheult, evidence suggests sun exposure may help combat any number of respiratory infections, including COVID, and the production of melatonin in your mitochondria appears to be a key part of why that works.
Seheult reviews a number of evidences showing that COVID rates across the world correlate to the solar index or the amount of sun striking the area. Positive case rates also correlate with vitamin D levels in the blood. Higher blood levels correlate with lower incidence of COVID and higher rates of survival for inpatients.
In short, vitamin D is more than likely a MARKER or surrogate for sun exposure. But all the benefits are likely due to other factors than vitamin D itself. As noted by Seheult, some studies looking at the effect of giving vitamin D to patients treated for severe COVID found no benefit, even at very high doses.
What’s more, research10 looking at UVA levels and COVID mortality rates found areas of the U.S., the U.K. and Italy with higher UVA also had lower COVID mortality rates. Vitamin D does not rise in response to UVA (only UVB), so, something in the sunlight, other than vitamin D, must have a beneficial impact. As noted by the authors:
“In conclusion, this study is observational and therefore any causal interpretation needs to be taken with caution. However, if the relationship identified proves to be causal, it suggests that optimizing sun exposure may be a possible public health intervention.
Given that the effect appears independent of a vitamin D pathway, it suggests possible new COVID-19 therapies and the importance of exploring the role of circulating NO [nitric oxide].”
Here, they speculated that nitric oxide, which is produced in response to UVA, could be the key, as nitric oxide has been shown to limit SARS-CoV-2 replication in vitro in addition to normalizing your blood pressure.
But while it’s true that nitric oxide rises in response to sunlight (specifically UVA and near-infrared), Seheult believes the primary mechanism at work here is melatonin, because it’s produced in response to the infrared spectrum, which makes up a much greater portion of the solar spectrum than ultraviolet, and works regardless of the angle at which it hits the earth.
Hence the southern part of England can have lower COVID deaths than the northern part, even though the entire country is too far north for vitamin D production.
Understanding Solar Energy
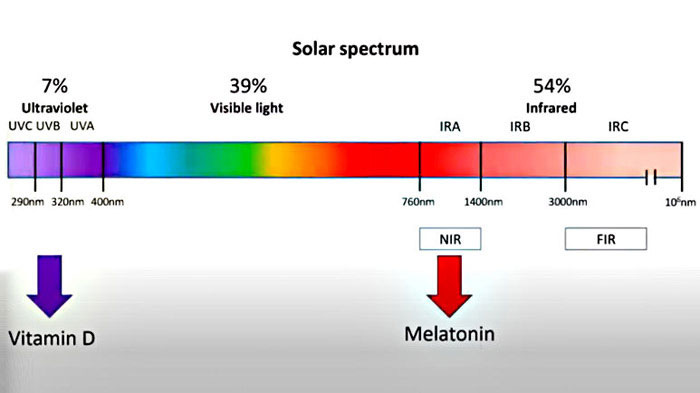
As you can see from the illustration above, 39% of the solar spectrum is what we see as visible light. The majority of the solar spectrum, 54%, is infrared,11 which is not visible but rather felt as heat. Ultraviolet light accounts for only 7% of the solar spectrum, and vitamin D is specifically produced in response to UVB radiation, which is only a small part of the ultraviolet spectrum.
Melatonin is produced inside your mitochondria in response to near-infrared radiation, which is part of the infrared spectrum. Because near-infrared has a much longer wavelength than ultraviolet, it can penetrate much deeper into your body, reaching cells in your subcutaneous tissue and not just on your skin. Near-infrared is not seen but rather felt as warmth. Its penetrative power (heat) also means it can penetrate lightweight clothing.
Melatonin Combats Oxidative Stress, Day and Night
Your mitochondria produce ATP, the energy currency of your cells. A byproduct of this ATP production are reactive oxidative species (ROS), which are responsible for oxidative stress. Excessive amounts of ROS will damage your mitochondria, contributing to suboptimal health, inflammation and chronic health conditions such as diabetes, obesity and thrombosis (blood clots).
The good news is your body has a built-in way to counteract these ROS. Inside your mitochondria, you also have an antioxidant system, and the main antioxidant is melatonin. (Melatonin also upregulates your glutathione pathway.)
“During the day, near-infrared rays from the sun penetrate deep into your body and activate cytochrome c oxidase, which in turn stimulates the production of melatonin inside your mitochondria.”
Melatonin is perhaps best known as a sleep regulating hormone. At night, the level produced by your pineal gland rises, which help make you sleepy and ready for bed. As the sun rises and morning dawns, the level automatically recedes, allowing you to wake up.
But that’s not all melatonin does. As melatonin is released at night, it travels through your circulatory system and is taken up by cells. Once inside, the melatonin mops up excessive ROS.
Melatonin also helps counteract damaging ROS during the day, but through a different pathway. During the day, near-infrared rays from the sun penetrate deep into your body and activate cytochrome c oxidase, which in turn stimulates the production of melatonin inside your mitochondria.
Melatonin and Sunlight Are Intimately Connected
Melatonin and sunlight are intimately linked and their relationship is unique in the fact that there are two forms of melatonin, circulatory and subcellular, or that produced by the pineal gland and secreted into the blood, and that produced by your mitochondria and used there locally.
Both appear to be controlled by either the absence of sunlight or the presence of sunlight. While circulatory melatonin may be the “hormone of darkness,” subcellular melatonin is the “hormone of daylight.”
Since the beginning of human history, people have lived and worked outdoors during the light of day, absorbing light energy from the sky. An average of 10 hours outdoors each day, 70 hours weekly, was common. Today, we spend an average of fewer than 30 minutes a day or a mere three hours per week in daylight, according to a study by Dr. Daniel Kripke, professor of psychiatry at UC San Diego.12
It is likely that near-infrared (IR) photons stimulate subcellular melatonin synthesis in your mitochondria through cyclic adenosine monophosphate (cAMP) or NF-kB activation, or alternatively by stimulating bone marrow stem cells.13 However, if you fail to expose your skin to sufficient near-IR light from the sun than your mitochondria will have seriously depleted melatonin levels that can’t be corrected through supplementation.
Melatonin’s Role in COVID
Alright, so what does all of this have to do with treating COVID? For this, we need to snake our way through some biology. Angiotensin 2 is a pro-oxidant that is converted into angiotensin 1,7, an antioxidant, by the ACE2 enzyme. ACE2 is the same enzyme the SARS-CoV-2 spike protein attaches to and uses to enter the cell.
Angiotensin 2 increases blood pressure while angiotensin 1,7 lowers it by relaxing your vasculature. If you have high angiotensin 2, you’ll have higher ROS in the cell, which, as mentioned is detrimental, as it damages the machinery of the cell. Angiotensin 1,7, on the other hand, will decrease ROS in the cell.
The problem you encounter with COVID is that when the virus attaches to the cell, it knocks out the ACE2 enzyme (because the spike protein is now bound to it). So, angiotensin 2 increases, angiotensin 1,7 decreases, and the conversion from angiotensin 2 to angiotensin 1,7 cannot occur.
As a result, ROS increases unchecked inside the cell. SARS-CoV-2 infection also increases white blood cell production, and that increases ROS as well. The end result of this elevated oxidative stress is blood clots, which in turn leads to hypoxemia.
Melatonin can break this destructive cycle by mopping up ROS and protecting your mitochondria from destruction.14 As noted by Seheult, if you’re not getting enough sleep at night, and not getting enough sun exposure during the day, your mitochondria are basically “running hot” with inflammation. Melatonin is the coolant that dampens the ROS in your mitochondria.
If your mitochondria are already taxed and you come down with COVID, the added stress can tip you over the edge. If your melatonin system is working well, because you’re getting good sleep and plenty of sun exposure, you’re more likely to fight off the infection and not have it turn serious.
Seed Oils Increase Your Risk for Both COVID and Sunburn
This may seem like a tangent, but it’s an important one. Linoleic acid (LA) makes up the bulk — about 60% to 80% — of the omega-6 fat you consume, and it’s a primary contributor to nearly all chronic diseases. While formerly thought an essential fat, when consumed in excessive amounts, LA actually acts as a metabolic poison.
At a molecular level, excess LA consumption damages your metabolism and impedes your body’s ability to generate energy in the mitochondria. Polyunsaturated fats such as LA are highly susceptible to oxidation, which means the fat breaks down into harmful subcomponents. Oxidized LA metabolites (OXLAMs) are what cause the damage.
Over the last 150 years, the LA in the human diet has increased from 2 to 3 grams a day to 30 or 40 grams. It used to make up just 1% to 2% of the energy in our diet and now it makes up 15% to 20%.This massive increase in LA consumption is what likely contributes to the increased oxidative stress in your body contributing to an increased risk for virtually every chronic degenerative disease.
Primary sources are seed oils and processed foods (which contain seed oils). Conventionally-raised chicken and pork are other common sources, thanks to the LA-rich grains they’re fed. As indicated in the subhead, high LA intake can raise both your risk for sunburn (which you don’t want as that’s what’s contributes to skin cancer) and your risk for COVID.
Eliminating seed oils from your diet will dramatically reduce your risk of sunburn and skin cancer, as susceptibility to UV radiation damage is controlled by the level of PUFAs in your diet. It’s almost like a dial. The PUFAs control how rapidly your skin burns, and how rapidly you develop skin cancer.
As for LA’s impact on COVID, consider this: The key toxin that produces the symptoms of acute respiratory distress syndrome (ARDS) is called leukotoxin, which is made from LA by white blood cells to kill pathogens. Basically, the white blood cells convert the LA into leukotoxin, which contributes to the inflammatory domino effect Seheult describes.
Leukocytes incubated with LA convert all of the LA into this toxin until there's none left, so, a major part of the disease process in ARDS is the conversion of LA into leukotoxin. That appears to be what’s killing many COVID patients. So, in summary, simply eliminating (or radically reducing) seed oils and conventional chicken and pork from your diet can go a long way toward:
Reducing your risk of sunburn, thus allowing you to get plenty of worry-free sun exposure to raise your vitamin D level, increase nitric oxide and boost melatonin production in your mitochondria
Lowering your risk of COVID complications by limiting the conversion of LA into leukotoxin
How Melatonin Is Created in Your Mitochondria
While Seheult focuses on the role of melatonin in COVID-19, the paper, “Melatonin in Mitochondria: Mitigating Clear and Present Dangers,”15 goes into much broader applications.
Again, melatonin is important for fighting cancer, and mitochondrial dysfunction plays a central role in most all chronic disease, including cancer, Parkinson’s, Alzheimer’s disease, heart disease and Type 2 diabetes, just to name a few. The paper also describes in far greater detail the mechanism for how melatonin is created within the mitochondria:16
“In normal cells, mitochondria account for energy (ATP) production, which results from glucose metabolism (glycolysis) and cellular respiration (oxidative phosphorylation or OXPHOS) in the inner mitochondrial membrane.
Glycolysis, which occurs in the cytosol, generates pyruvate, which is actively transported into the mitochondrial matrix. Here, pyruvate is converted to acetyl-CoA, the latter linking glycolysis with the citric acid cycle in the mitochondrial matrix and thus coupling it to ATP production.
Acetyl-CoA is also an essential co-factor for N-acetyltransferase (AANAT), which converts serotonin to N-acetylserotonin, the precursor of melatonin; AANAT activity rate limits melatonin synthesis.
In contrast to normal cells, many solid tumor cells allow the metabolism of glucose to pyruvate in the cytosol but restricts the transfer of pyruvate into the mitochondria; this is known as the Warburg effect ... The Warburg effect allows cancer cells to rapidly proliferate, avoid apoptosis, and enhance the invasiveness and metastatic processes characteristic of tumors.”
The Warburg Effect in COVID
Interestingly, the Warburg effect is also at play in COVID. As explained in a June 2020 study17 that found melatonin inhibited COVID-19-induced cytokine storm, when your immune cells are in a hyper-inflammatory state, their metabolism changes in a way similar to that of cancer cells:
“Similar to cancer cells … immune cells such as macrophages/monocytes under inflammatory conditions abandon mitochondrial oxidative phosphorylation for ATP production in favor of cytosolic aerobic glycolysis (also known as the Warburg effect) …
The change to aerobic glycolysis allows immune cells to become highly phagocytic, accelerate ATP production, intensify their oxidative burst and to provide the abundant metabolic precursors required for enhanced cellular proliferation and increased synthesis and release of cytokines ...
Because of melatonin's potent antioxidant and anti-inflammatory activities, it would normally reduce the highly proinflammatory cytokine storm and neutralize the generated free radicals thereby preserving cellular integrity and preventing lung damage.”
Optimize Your Health With Sensible Sun Exposure
Basically, what “Melatonin in Mitochondria” found is that melatonin is an ideal target when trying to combat mitochondria-related diseases and cancer, because it has ready access to, and is synthesized in, your mitochondria, right where the oxidative stress occurs. By reprogramming the faulty glucose metabolism, melatonin can optimize mitochondrial function and curtail cancer growth.
Remember, taking melatonin supplements will not transfer to increasing mitochondrial melatonin production. It needs to be produced near your mitochondria and not float down from your pineal gland. So, oral supplementation is not a substitute for going outside during the day.
If you take it during the day, you’re tricking your body into thinking it’s nighttime, which could cause problems. As far as we know, the best way to increase mitochondrial melatonin is to optimize your near-IR exposure through regular sunlight exposure.
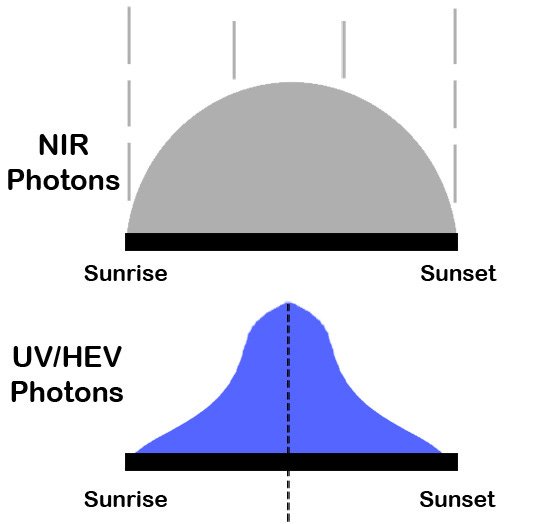
As you can see in the graph above, unlike increasing vitamin D, you have a much broader window where you can get near-IR exposure. Interestingly, spending time in nature is another way to increase your IR levels as most green plants and trees reflect IR. This is likely why forest bathing is so healthy.
The good news is you don’t have to be close to naked to benefit, as you do when optimizing your vitamin D production. The near-infrared radiation will penetrate lightweight clothing. So, you can cover yourself to prevent sunburn if you’re outside for a longer period of time, while still getting the near-infrared that you need. (Also, remember what I just told you about eliminating LA from your diet to cut your sunburn risk.) That said, you will absorb more IR on your bare skin.
The other side of the equation is avoiding bright light late at night. To optimize melatonin release in your pineal gland at night, avoid blue light-emitting gadgets at least a couple of hours before bed and keep the lighting in your room dim. Blue-blocking glasses can also be used. Once in bed, makes sure your room is pitch black, as even a small amount of light can interfere with melatonin production.
Together, sun exposure during the day and keeping it dark at night, will ensure your mitochondria are being bathed — day and night — in melatonin that reduces harmful ROS. So, as suggested by Seheult, try to spend more time outdoors, especially if you’re sick (whether it be COVID or some other respiratory infection) or battle chronic disease.
Access this content 48 hours faster by subscribing to the FREE Mercola Health Newsletter today.
Disclaimer: The entire contents of this website are based upon the opinions of Dr. Mercola, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked.
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Mercola and his community. Dr. Mercola encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. The subscription fee being requested is for access to the articles and information posted on this site, and is not being paid for any individual medical advice.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.