Natural Therapies for Cystic Fibrosis
Cystic fibrosis is a progressive and terminal disease characterized by an overproduction and buildup of thick mucus in the lungs and other organs.
STORY AT-A-GLANCE
Cystic fibrosis (CF) is a severe genetic disorder marked by excessive, thick mucus in the lungs and other organs, leading to chronic inflammation and reduced lung function, necessitating daily breathing treatments
Nutritional support, including vitamins A, C, E, zinc, omega-3 (DHA), garlic, ginseng and curcumin, is commonly recommended for CF patients
Vitamin D deficiency is notably prevalent among CF patients, affecting their lung function and overall disease progression; maintaining a vitamin D level of at least 60 ng/mL is recommended for mitigating these effects
N-acetylcysteine (NAC) has emerged as a significant antioxidant in CF management, helping to reduce inflammation, break down mucus, enhance antibiotic effectiveness, and support immune response
Reducing dietary intake of linoleic acid (LA) is advised for CF patients due to its potential to exacerbate disease symptoms through mitochondrial dysfunction
Cystic fibrosis (CF) is a progressive and terminal genetic disease that causes an overproduction and buildup of thick, sticky mucus in the lungs and other organs that lead to chronic inflammation and, eventually, a deterioration of lung function.
The disease requires daily breathing treatment for up to five hours a day, and many CF patients end up spending a lot of time in the hospital due to respiratory distress and chronic infections. Pancreatic and gastrointestinal complications, including malabsorption of proteins and fats, and chronic liver disease are also common. The median survival age is about 35 years.1
A 2012 paper2 in the Journal of Pharmacy Practice reviewed several of the most commonly recommended nutritional supports for those with CF, including vitamins A, C and E, zinc, omega-3 docosahexaenoic (DHA), garlic, ginseng and curcumin.
According to this paper, 75% of CF patients routinely use complementary and alternative medicine (CAM) in addition to their regular treatment, so it’s important for health professionals to be familiar with these options.
More recently, a scientific review3 published in 2022 highlighted the role of N-acetylcysteine (NAC) in the clinical management of CF. Removing all linoleic acid (LA) from your diet and optimizing your vitamin D level are two additional foundational recommendations that I will go over here.
Vitamins A, C and E and Zinc
Many CF patients have poor absorption of fat-soluble vitamins such as A and E, due to malabsorption of fats. For this reason, supplementation with these vitamins is often recommended. As a rule, patients are advised to consume between 120% and 150% of the recommended daily allowance (RDA) of nutrients to prevent premature death from malnutrition.4
The Journal of Pharmacy Practice paper5 cites research from 2001, which found that CF patients who received 1 milligram of beta-carotene per kilo of bodyweight per day (up to 50 mg per day) for three months, followed by a daily dose of 10 mg for another three months, experienced “a statistically significant decrease in the number of days of treatment with systemic antibiotics.”
Zinc supplementation at a dose of 30 mg per day has also been shown to reduce the average days of antibiotic use, and a pediatric study using an antioxidant-rich multivitamin supplement containing vitamins A, C, E and zinc and other micronutrients found “modest improvement” in lung function.
How to Select a Good Vitamin Supplement
Vitamin A (retinol) should not be confused with beta-carotene, which is pre-vitamin A that gets converted into vitamin A in your liver. To use beta-carotene, you need to have a well-functioning digestive tract and sufficient bile produced by your gallbladder. Specific enzymes are also needed to break down the carotene for the conversion into retinol to occur.
Most people have poor gut health, and this is particularly true for CF patients, which makes beta-carotene a poor alternative as a primary source of vitamin A. Retinol — preformed vitamin A — is found in animal products such as grass fed meat and poultry, liver, fish and raw organic dairy products like butter. This is the form of vitamin A your body can use, so make sure the vitamin A you buy specifies “retinol” or “retinoic acid,” and not just “vitamin A” or “beta-carotene.”
When it comes to vitamin C, you want to make sure it’s liposomal, as it will allow you to take higher dosages without causing loose stools. It’s also absorbed better.
While healthy people can typically get enough vitamin C from food such as red pepper, broccoli, kiwi, strawberries, citrus fruits, camu camu, rose hips or acerola cherries, if you’re ill, you need far more than what can be obtained from food (possibly except for acerola cherry, which contains 80 mg of vitamin C per cherry).
Selecting a natural supplement is particularly important when it comes to vitamin E. Studies have demonstrated that synthetic vitamin E has the opposite effect of natural vitamin E, such as increasing the risk of certain cancers rather than lowering it,6 7 8 for example. So, it’s important to make sure you’re getting a natural version.
What you’re looking for is “d alpha tocopherol.” Avoid all synthetic forms such as succinate, acetate and the racemic DL isomer. You want the pure D isomer, which is what your body can use. There are also other vitamin E isomers, and you want the complete spectrum of tocotrienols, specifically the beta, gamma, and delta types of vitamin E, in the effective D isomer.
Vitamin D
Vitamin D also plays a crucial role in the health and management of CF, offering several benefits backed by scientific research. A systematic review and meta-analysis9 published in January 2024 revealed that CF patients typically have significantly lower levels of vitamin D compared to healthy controls, both in childhood/adolescence and adulthood.
The prevalence of vitamin D levels considered insufficient (20–30 ng/mL) in CF patients was found to be 36% among pediatrics and adolescents and 63% among adults. Twenty-seven percent of pediatric/adolescent CF patients and 35% of adults had vitamin D levels of below 20 ng/mL, which is a severe deficiency state.
Ideally, you’d want a vitamin D level of at least 60 ng/mL year-round. To reach that level, I recommend daily walks with minimal clothing for 30 minutes before and after solar noon, for a total of one hour. During summertime, that would be right around 1 pm.
While oral vitamin D3 supplementation is an option if you cannot get enough sun exposure, you’ll miss out on many of the other health benefits that sun exposure provides. You also need to make sure you’re taking vitamin K2 and magnesium when using oral supplementation.
How Vitamin D Deficiency Impacts CF
Another study10 focused on the relationship between vitamin D levels and lung function in CF patients, specifically through the lung clearance index (LCI), a measure of lung function. The study found a strong negative correlation between vitamin D levels and LCI, indicating that lower vitamin D levels are associated with worse lung function.
It also noted that vitamin D deficiency could be particularly detrimental in patients with comorbidities such as cystic fibrosis-related diabetes (CFRD) and cystic fibrosis liver disease (CFLD).
Additionally, a pilot study11 published in 2019 investigated the immunomodulatory effects of vitamin D on pro-inflammatory cytokines in the airways of CF patients infected by Pseudomonas aeruginosa.
They found that supplementation with vitamin D led to a decrease in the levels of interleukins IL-17A and IL-23 in the exhaled breath condensate (EBC), indicating a reduction in inflammation.
These cytokines are known to play roles in the body's inflammatory response, suggesting that vitamin D supplementation can help modulate the immune response in CF patients, potentially mitigating lung damage caused by chronic infections.
These findings collectively underscore the importance of monitoring and managing vitamin D levels in CF patients, not only for bone health but also for its potential benefits in improving lung function, reducing inflammation, and enhancing the body's response to infections.
N-acetylcysteine (NAC)
NAC is a precursor to your body’s production of glutathione (GSH), also has an important role in the management of CF.12 As noted in the journal Pharmaceuticals:13
“[NAC] has been known for a long time as a powerful antioxidant and as an antidote for paracetamol overdose. However, other activities related to this molecule have been discovered over the years, making it a promising drug for diseases such as cystic fibrosis (CF).
Its antioxidant activity plays a key role in CF airway inflammation and redox imbalance. Furthermore, this molecule appears to play an important role in the prevention and eradication of biofilms resulting from CF airway infections, in particular that of Pseudomonas aeruginosa …
To do this, NAC can act alone, but it can also be used as an adjuvant molecule to known drugs (antibiotics/anti-inflammatories) to increase their activity.”
Here’s a quick overview of how NAC can be beneficial for CF patients, drawing on its various mechanisms:14
Fighting oxidative stress — There's a battle between damaging oxidative substances (ROS) and the body's antioxidants. NAC steps in as a reinforcement, helping to boost the body's antioxidant levels, especially glutathione (GSH). This helps to mitigate the damage caused by oxidative stress, which can worsen CF conditions.
Reducing inflammation — CF lungs are often inflamed, partly due to overactive immune responses that attract too many neutrophils (a type of white blood cell) to the site. These neutrophils release substances that can damage lung tissue. NAC helps calm this overreaction, reducing inflammation by modulating the production of molecules like cytokines that drive the inflammatory process.
Breaking down mucus — The thick mucus in CF can trap bacteria, creating biofilms that are hard to treat. NAC can break the sulfur bonds in the mucus, making it less sticky and easier to clear from the lungs. This action helps disrupt the biofilm structure, allowing antibiotics to reach and kill bacteria more effectively.
Enhancing antibiotic effectiveness — The presence of biofilms and thick mucus in CF lungs can make bacteria resistant to antibiotics. NAC can make these bacteria more susceptible to antibiotics by breaking down the biofilms. It can also work synergistically with certain antibiotics, improving their ability to kill bacteria.
Acting against bacteria directly — Even though NAC is not an antibiotic, it has properties that can directly inhibit the growth of bacteria and their ability to form biofilms. This adds an extra layer of defense against lung infections.
Supporting healthy immune responses — By reducing the oxidative stress and helping to manage the inflammatory response, NAC can indirectly support the body's immune system, making it more effective at fighting off infections without causing additional damage to lung tissues.
Improving cell function — On a cellular level, NAC might help correct some of the dysfunction caused by the CF mutation. It has been suggested that NAC can help with the maturation and function of CFTR proteins, which are faulty in CF, thereby helping to alleviate some of the symptoms.
Omega-3
Omega-3 is also thought to be important for CF patients because deficiency has been linked to worsened pulmonary and GI symptoms, as well as CF progression. DHA, in particular, is important, as it has a beneficial impact on lung function. Previous research has concluded that doses up to 50 mg of DHA per kilo of bodyweight is safe for CF patients.15
When it comes to omega-3, I recommend trying to get most of it from omega-3-rich seafood, such as wild-caught Alaskan salmon, herring, sardines, mackerel and anchovies. If using a supplement, avoid synthetic fish oils and opt for krill oil instead.
Herbal Remedies
Herbal remedies recommended for CF include:16
Garlic, which has antibacterial effects.
Ginseng, which has antioxidant, antimicrobial and immune modulating effects. Aqueous extract of ginseng has been shown to be effective in inhibiting P aeruginosa, a bacteria often involved in chronic pulmonary infections, including antibiotic-resistant strains.
Curcumin, which has antioxidant properties. Limited data also suggests it may increase CFTR-regulated channel activity in CF patients. CFTR is a protein that, when dysfunctional, results in the development of CF symptoms.
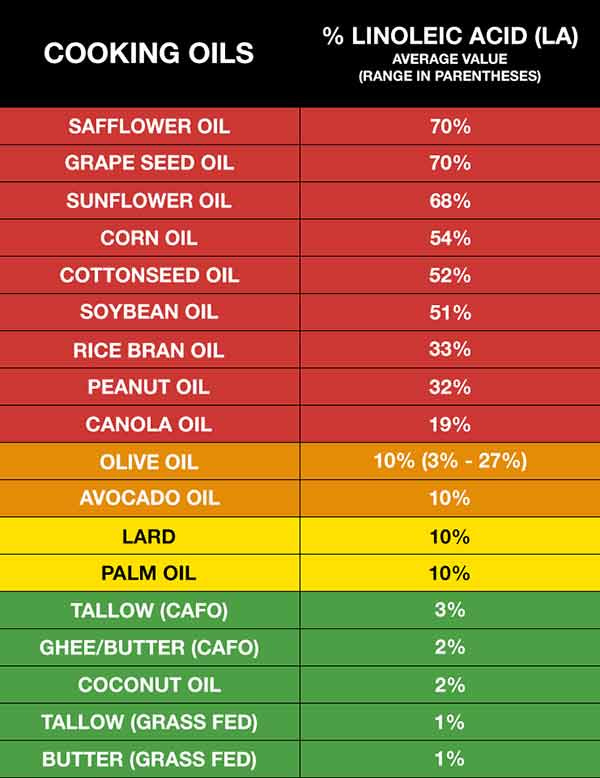
Eliminate Linoleic Acid From Your Diet
As important as supplementing certain nutrients might be, CF patients must also be vigilant about avoiding certain things. As explained in my in-depth review, “Linoleic Acid — The Most Destructive Ingredient in Your Diet,” linoleic acid (LA) — an omega-6 polyunsaturated fat (PUFA) — acts as a mitochondrial poison and the primary contributor to all chronic disease.
If you have CF, I strongly advise you to eliminate as much LA from your diet as humanly possible. While LA is found in most foods, by eliminating processed foods, condiments, seed oils for cooking, fast food and restaurant food, and conventionally raised pork, chicken and eggs, you can get your LA intake below 5% of daily calories, which is about what our ancestors used to get.
While there are no studies detailing direct harm caused by LA in CF, dysfunctional lipid metabolism, including LA metabolism, is a characteristic of CF. So, there appears to be a complex interaction with LA that could influence disease outcomes.
“Excess LA is a primary driver of mitochondrial dysfunction, and well-functioning mitochondria are a prerequisite for health and disease prevention.”
That said, considering excess LA is a primary driver of mitochondrial dysfunction, there’s every reason to believe that it will have a detrimental impact on CF. After all, health and disease prevention require you to have well-functioning mitochondria. It’s as foundational as you can get.
If you’re not sure how much you’re eating, enter your food intake into Cronometer — a free online nutrition tracker — and it will provide you with your total LA intake. Cronometer will tell you how much omega-6 you're getting from your food down to the 10th of a gram, and you can assume 90% of that is LA. Anything over 10 grams of LA is likely to cause problems.
Healthy fat replacements include tallow, butter or ghee, all of which are excellent for cooking. The table below provides a fairly comprehensive list of the most commonly consumed oils and their approximate LA content.
In general, the lowest LA-containing fats — butter and beef tallow — would be the fats of choice. These excellent cooking fats would not only be the lowest in LA, but will also provide the fat-soluble vitamins, A, D, and K2. Coconut oil is also very low in LA but doesn’t provide the important fat-soluble vitamins that tallow and butter contain.
Vitamin E Prevents Oxidation of LA
If you’ve been eating a high-PUFA diet for a long time, consider taking vitamin E regularly until you get your LA down to healthy levels. As noted earlier, CF patients need extra vitamin E anyway, and this is yet another reason to make sure you’re getting enough.
High LA levels increase a potentially dangerous process in your body called lipolysis — the liberation of fatty acids from your fat cells into your bloodstream where they are mobilized. This then increases the oxidation of LA, which is precisely what you want to avoid. Ideally, you want to keep LA in your fat cells until they metabolize it with peroxisomes. Vitamin E can help neutralize this damaging effect of LA.
Due to the high LA burden, few people can get enough vitamin E from their diet to suppress the oxidative destruction caused by LA unless they're supplementing with vitamin E.
The good news is that since the supplementation is short term, you're not going to need it the rest of your life. If you can keep your LA intake to below 5 grams a day for three years, it's likely you may not even need it at all, or at most, only a few times a month.
The Story of Claire Wineland
Claire Wineland, an inspirational speaker and YouTube sensation, was diagnosed with CF at birth. At age 13, she founded the Claire’s Place Foundation17 to help families with children who have CF. She died September 2, 2018, from a massive stroke following an otherwise successful lung transplant.
In 2016, Wineland appeared in an episode of “My Last Days,” a limited CW docuseries hosted by Justin Baldoni, featuring people living with terminal illness. September 2, 2019, YouTube Originals released the documentary “CLAIRE,” directed by Nicholas Reed (above).
While filled with chronic illness, Wineland’s life was a testament to how to live life well, with purpose and gratitude. It’s a potent reminder of how we need to live life to the fullest, even though we might die tomorrow. “I’ve always loved the idea of bringing life into places where people think life doesn’t really exist,” Wineland said.
Wineland’s mother said she was convinced her daughter came into the world with a mission to share the message of “what it’s like to be blessed with life.” I couldn’t agree more.
Disclaimer: The entire contents of this website are based upon the opinions of Dr. Mercola, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked.
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Mercola and his community. Dr. Mercola encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. The subscription fee being requested is for access to the articles and information posted on this site, and is not being paid for any individual medical advice.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.





Report with excellent remedies for cystic fibrosis. Cystic fibrosis is a multisystem autosomal recessive genetic disorder that affects the lungs, and to a lesser extent the pancreas, liver and intestine. Cystic fibrosis affects more than 30,000 children and young adults in the U.S. Cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD) are chronic lung diseases that affect an estimated 70,000 to 251 million people worldwide. world, respectively. Although these two diseases have clearly different pathophysiologies, both cause chronic respiratory failure that erodes quality of life.
Advanced Functional Medicine has experience supporting people with this chronic disease. Assessing intestinal function and intestinal permeability, optimizing the immune system, supporting mucous membranes, and balancing mineral deficiency are effective strategies that have helped patients improve quality of life. Studies show that by improving these systems patients' symptoms can improve greatly.
1) Increase mucolytic foods: garlic, onion, watercress, horseradish, mustard, parsley, celery, rose hip tea, pickles, lemons.
2) Emphasize anti-inflammatory foods: cold water oily fish, berries and seeds, turmeric, ginger, green tea, low omega 6 olive oil.
3) Emphasize foods rich in antioxidants to support immune function: berries, green tea, turmeric, fruits and vegetables.
4) Minimize pro-inflammatory foods: sugar, refined carbohydrates, trans fats, excess commercially produced red meat, omega-6 fatty acids, caffeine and alcohol.
5) Help avoid fat-soluble vitamin deficiencies by taking daily amounts of vitamin A, vitamin D, and vitamin E and K,
6) Include foods rich in vitamin C and quercetin: for example, berries, cherries, citrus fruits, apples, onions, parsley, black and green tea, kale and broccoli.
Supplements that support cystic fibrosis
1) N-acetylcysteine (NAC) inhaled or oral. NAC can regulate cell apoptosis, angiogenesis, growth arrest, redox reaction, and inflammatory responses. High-dose NAC has anti-inflammatory benefits and improvements in aspects of quality of life and measures of lung function. It is safe and well tolerated.
2) Vitamin C and bioflavonoids: anti-inflammatories, antioxidants and immune support.
3) Zinc
4) Garlic Supplement: Broad Spectrum Antibiotic and Mucolytic
5) Digestive enzymes with meals.
6) Omega-3: anti-inflammatories
7) Broad spectrum antioxidants: beta-carotene, vitamin E, selenium, coQ10
8) Protein supplementation may be necessary in hypoproteinemia.
Herbal Medicine Treatment That Supports Cystic Fibrosis
1) Immune Support: Echinacea, Andrographis, Olive Leaf, Siberian Ginseng, Reishi/Shitake
2) Expectorants: thyme, elecampane, mullein, licorice, anise, hyssop, cayenne.
3) Mucous tonics: goldenseal, eyebright
4) Bitters (digestive, pancreatic and liver function): gentian, fringe tree, dandelion, blue flag
5) Antimicrobials: goldenseal, echinacea, thyme, wild indigo
6) Anti-inflammatory: boswellia, turmeric, ginger.
7) Antioxidants: turmeric, green tea, rosemary, grape seed, Santa María thistle.
https://advancedfunctionalmedicine.com.au/cystic-fibrosis-symptoms-causes-natural-treatment/ .----
https://pubmed.ncbi.nlm.nih.gov/30627668/ (2018).--
https://www.mdpi.com/1424-8247/15/2/217 (2022).-
https://www.mdpi.com/2076-3921/12/9/1713 (2023).--
https://journals.lww.com/rips/fulltext/2023/18020/N_Acetylcysteine_attenuated_pulmonary_fibrosis.6.aspx (2023).--
https://www.sciencedirect.com/science/article/abs/pii/S1094553923000950 (2024).--
https://journals.sagepub.com/doi/full/10.1177/17534666231158563 (2024).--
https://draxe.com/health/cystic-fibrosis/ .---
https://www.peacehealth.org/medical-topics/id/hn-1199008 .----
https://ijpjournal.com/wp-content/uploads/2021/05/2-Vol.-8-Issue-3-Mar-2021-IJP-RE-318.pdf (2021).--
Thank you Dr. Mercola for addressing CF with so many clear ways to fight this disease. Many of the supplements my daughter takes already but this confirms and helps to know what to add and how much. Also it is not just me trying to tell her what to take she can now read a succinct article to reference for herself. I am very grateful to you for writing this - thank you!