What Everyone Needs to Know About Antidepressants
The most common harm isn't always obvious at first - it can look like 'you,' feel like relapse, or show up as strange new symptoms that quietly pull people into a cycle that's hard to reverse.
STORY AT-A-GLANCE
SSRI antidepressants are one of the most harmful medications on the market, and because of just how many people they are given to (often for no good reason as only a minority of patients benefit from SSRIs) they have had a profound effect on the consciousness of our entire society
This article will review some of the more common side effects of SSRIs (and SNRIs), such as losing the ability to have sex, becoming numb to life, becoming severely agitated or imbalanced (sometimes to the point one becomes violently psychotic or commits suicide), losing your mind, and the development of birth defects
Like many other stimulant drugs (e.g., cocaine) SSRIs can be very difficult to quit. Because of this, patients frequently get severely ill when they attempt to stop them (withdrawals affect roughly half of SSRI users). Worse still, it is often extremely difficult to withdraw from them and very few doctors know how to safely facilitate this
Due to widespread denial in psychiatry about the issues with their drugs the common SSRI side effects (e.g., withdrawals) are often misinterpreted as a sign the individual had a pre-existing mental illness and needs more of the drug — which all too often then leads to catastrophic events for the over-medicated patient
This article will provide the critical information SSRI patients are rarely warned about and resources for patients already trapped in challenging mental health situations
The public is at last awakening to the dirty secret of SSRI antidepressants — they trigger psychotic violence (e.g., suicides and sometimes mass shootings). This side effect was discovered in clinical trials but covered up by the FDA, even after the agency received a deluge of complaints (39,000 in the first nine years1) once the first SSRI, Prozac, hit the market. For example, consider how they acted at this 1991 Congressional hearing:
Because of those deaths, lawsuits through discovery found the drug companies were well aware of these issues (and many more) but chose to conceal them. As such, we now have a much clearer picture of the harms of these medications.
Note: While many patients react badly to SSRIs, there is also a subset of patients who benefit from SSRI antidepressants (discussed here). Sadly, it is quite rare that patients will work with antidepressant prescriber practitioners who have the time and knowledge to accurately determine which patients to give these drugs to.
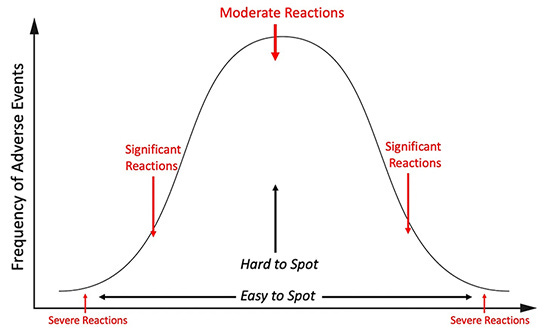
The Toxicology Bell Curve
In toxicology, you will typically see severe and extreme reactions occur much less frequently than moderate reactions:
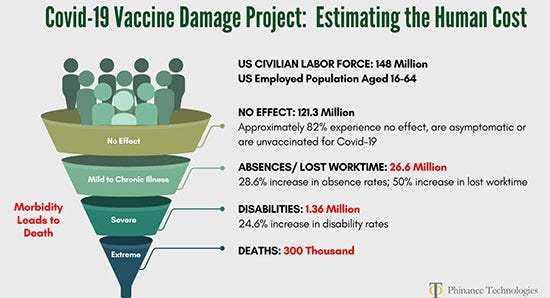
For example, consider the distribution of injuries from the COVID-19 vaccines.
Note: These calculations were based on 2023 data,2 and since then, vastly more evidence of harm has emerged (e.g., a recent poll found 63 million American adults had minor reactions to the vaccine and 17 million had severe side effects3).
As such, violent psychosis is just the tip of the iceberg for the mind-altering effects SSRIs have. For example, in a survey of 1,829 patients on antidepressants in New Zealand:4
62% reported sexual difficulties
60% felt emotionally numb
52% felt not like themselves
47% had experienced agitation
39% cared less about others
Most importantly, the respondents to that survey reported that their prescribers did not warn them about many of these side effects.
Doctored Data
Originally developed as a weight loss drug, Eli Lilly pivoted to having Prozac “treat” depression as this metric was subjective to the point any trial could be doctored to show a “benefit.” Despite this, Prozac’s initial data was so atrocious, it could only be approved through bribes (which a former Eli Lilly executive testified occurred).
This fraud is proven by patients consistently choosing to stop taking SSRIs despite them being “proven” to make you feel better:
A review of 29 published and 11 unpublished Paxil clinical trials containing 3,704 patients who received Paxil and 2,687 who received a placebo, an equal proportion of patients in both groups left their study early (suggesting Paxil’s benefits did not outweigh its side effects), and that compared to placebo, 77% more stopped the drug because of side effects and 155% more stopped because they experienced suicidal tendencies.5
A study of 7,525 patients found that 56% of them chose to stop taking an SSRI within 4 months of being prescribed it.6
An international survey of 3,516 people from 14 patient advocacy groups found that 44% had permanently stopped taking a psychiatric drug due to its side effects.7
A survey of 500 patients found 81.5% were unsure if their antidepressants were necessary.8
Note: Fluorinated versions of pharmaceuticals tend to be more toxic and persist for longer periods in the body (making them much harder to detoxify from). Many believe a key reason SSRIs cause so many issues is due to the high dose of fluoride they bring into the brain.
Violent Behavior
In 1985 when the FDA’s safety reviewer scrutinized Eli Lilly’s Prozac application, they realized Lilly had “failed” to report psychotic episodes of people on the drug and that Prozac’s adverse effects resembled that of a stimulant drug.
In turn, the warnings on the labels for SSRIs, such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and mania match the effects commonly observed with stimulant street drugs such as cocaine and methamphetamine.9 Likewise:
A Cochrane review found SSRIs were found to double the risk of suicide.10
A 2000 study of 20 volunteers in good mental health found Zoloft made 10% become suicidal (with one almost killing themselves) — both of whom remained deeply disturbed for months.11
Eli Lilly showed in 1978 that cats who had been friendly for years began to growl and hiss on Prozac and became distinctly unfriendly until Prozac was stopped.12
To illustrate what this can look like, I will share what four different patients experienced prior to killing themselves or others:13
“A month later, Toran experienced a severe cluster of adverse reactions including suicidal behavior, self-harm, aggression, hostility, hallucinations, lack of concentration and impaired functioning. The symptoms were so severe that he dropped out of school. His psychiatrist’s response was to increase his dose, which worsened the adverse reactions.
Six days later, Jake had his first reaction. He walked out of an exam half-way through it and cried for about 2-3 hours that night, saying, ‘You don’t know what it’s like in my head.’ His parents thought this was from the stress of the exams. They never imagined that a drug could do this to a person.
The last two days she was just a complete zombie I have to say. She was just agitated, jumping at every noise and not making sense. I was very concerned. We were very close to Cecily. I just loved her deeply.
Shortly before his death, Woody came home crying after driving around all day. He sat in a fetal position on the kitchen floor profusely sweating with his hands pressing around his head saying, ‘Help me. Help me. I don’t know what’s happening to me. I am losing my mind. It’s like my head is outside my body looking in.’”
Note: The process through which SSRIs do this (e.g., some individuals report an experience akin to “being possessed”) is discussed further here.
Fortunately, thanks to MAHA being elected to office, after decades, there at last appears to be real interest in addressing this issue. Consider, for example, this recent statement from H.H.S. Secretary Robert F. Kennedy Jr.:
Note: Initially, the media disclosed school shooters were on SSRIs, but then stopped ever mentioning a shooter’s medications. Recently, I learned through a CDC employee the CDC has found shooters continue to be on SSRIs but has avoided disclosing it to avoid the political ramifications of acknowledging this.
Likewise, the agitating quality of SSRIs can frequently trigger Bipolar disorder. For example:
Yale researchers reviewing the records of 87,290 patients with depression or anxiety found SSRIs made 7.7% become bipolar each year (tripling the rate patients become bipolar).14
A survey found 60% of bipolar patients become bipolar after receiving SSRIs for depression.15
Peter Breggin reported that of 184 hospitalized patients started on an SSRI, 11 developed mania and 8 became psychotic, and in Yale, 8% of 533 consecutive admissions were for mania or psychosis caused by antidepressants, with two patients heard voices commanding them to kill themselves.16
This helps to explain why bipolar has become hundreds of times more common since the pre-SSRI era and switched from being a temporary to lifelong condition that is far more disruptive and difficult to treat (e.g., 83% of bipolar patients reported being severely impaired in some facet of their lives).17 18
Note: A good case can be made that many of the severe complications from bipolar disorder are a result of the medications used to treat it rather than the disease itself.
Sexual Dysfunction
One of the most common ways antidepressants worsen depression is by causing permanent sexual dysfunction. For example, a Spanish study of five of the most commonly prescribed SSRIs found on average the drugs caused sexual disturbances in 59% of 1,022 (previously normal) patients, two-thirds of whom considered that dysfunction unacceptable and that:19 20
57% experienced decreased libido
57% experienced delayed orgasm or ejaculation
46% experienced no orgasm or ejaculation
31% experienced erectile dysfunction or decreased vaginal lubrication
Remarkably, to avoid scaring patients away from a “necessary” prescription, doctors rarely warn their patients of these side effects. Fortunately, two months ago, the New York Times finally brought mainstream attention to this and exposed that virtually no psychiatrist will disclose this issue to patients.21 To quote the article:
“Only over the past few years has Ruth learned, from her daughter, about the sexual side effects she still lives with and about her grief. ‘Her erogenous zones don’t work,’ ‘I have huge, terrible regret’ about allowing her child to be medicated. ‘I can’t believe I so easily said yes.’
He took a moderate dose, a 10 milligram pill, and an hour later, he said, ‘I had numb genitals.’ He abandoned the drug almost right away and has taken no psychiatric medication since. ‘Three years later,’ he explained, his penis ‘feels like my elbow — if you touch my elbow, it’s that same kind of sensation.’
And there is emotional numbness to go with the physical. ‘I can’t feel any connection to you guys — I feel like my soul was ripped out of my body.’ He has tried to get doctors to pay attention. ‘They were like: That’s impossible. It’s all in your head.’
But she noticed quickly that on the drug, climaxes became ‘superficial’ and ‘so short-lived,’ she recalled. ‘It infused a dominant emotion of frustration into sex.’ Her capacity for transporting sex is still mostly relegated to the past, and she worries that it will stay back there forever.
It has been six years since Guin stopped taking her S.S.R.I. She is 29. ‘I don’t have the capacity for romantic relationships,’ she said. ‘That’s just gone in a stark way. For me, the chemical mechanisms of the romantic are too deeply tied in with sexuality for the romantic to exist independently ... She has just had her first child.
Because she has no partner, she used in vitro fertilization.’ ‘I wanted a partner,’ she said. ‘I wanted a child to grow up with their mom and dad. Your sexual life is so core when you consider that the sexual relationship is the basis for most long-term relationships.’”
Emotional Anesthesia
Much in the same way SSRIs make you “sexually numb” they can do the same to emotions. Common stories include:
Losing the drive to exit a toxic situation (e.g., a relationship or job) and wasting years if not decades in it.
Losing the joy one felt in life.
Losing the depth and richness of life.
Note: In psychiatry, this effect is termed “emotional blunting,” and the studies I’ve reviewed found 40% to 60% of SSRI users experience this.
Worse still, SSRIs can also cause a variety of other disconcerting psychiatric changes (e.g., many report it feeling as though they are losing their mind).
Birth Defects
To increase sales, SSRIs are routinely pushed on pregnant mothers despite the fact:
SSRIs increase the risk of premature births, with the greatest risk (a doubling) occurring if an SSRI is taken during the third trimester.22
SSRIs significantly increase the risk of septal defects (which often require heart surgery to repair). One study of 500,000 Danish infants found taking a single SSRI while pregnant caused the likelihood of the child having one to go from 0.5% to 0.9% while taking two or more increased it to 2.1% (with the worst SSRIs tripling the risk).23
SSRIs significantly increase the risk of persistent pulmonary hypertension in a newborn baby. One study of 1,173 infants found SSRIs increased the risk of persistent pulmonary hypertension by 6.1 times,24 while another found a 4.29X increase25 and a third found a 2.5X increase.26
Note: Other newborn complications linked to SSRIs include irritability, tremor, hypertonia and difficulty sleeping or breastfeeding, along with reduced growth early in life.
SSRI Withdrawals
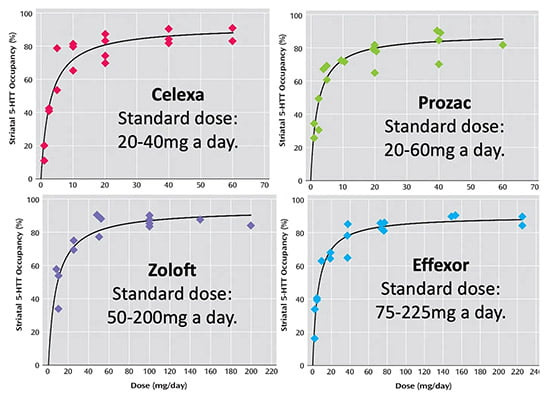
One of the most insidious aspects of SSRIs is that they are dosed so that you can easily enter severe withdrawals if you change their dose.27 28
This is immensely unfortunate as:
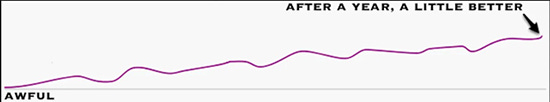
To “cure” an SSRI dependence (which is analogous to an addiction), you need to let the brain rewire itself back to normal, and until that happens, the brain will behave in an abnormal fashion (e.g., its ability to adapt to outside stressors in a healthy way is dramatically reduced). Since this is often a very slow back and forth process, the journey patients go through is frequently something like this as the brain tries to rewire itself:
It’s very hard to quit the drugs without triggering withdrawals, as in many cases, minuscule drops must be made over months (e.g., by lightly sanding off part of a pill slightly more each week), with the entire withdrawal process typically taking years — particularly since psychiatric patients tend to be on so many drugs (which are often given to manage the consequences of other medications) — and typically only one can be withdrawn from at a time.
These withdrawals are often quite severe, and in many cases, a SSRI dose change (either an increase or decrease) has been linked to violent or suicidal behavior.
Physicians typically interpret these withdrawals as proof “the medication was working and needs to be continued” because they chose to believe the SSRI was keeping an existing mental disease in check rather than causing severe psychiatric destabilization. As such, much like the bipolar example, when SSRIs create withdrawal issues, rather than recognize it, they will typically prescribe psychiatric medications to manage the new issues.
When people read other people’s stories, they realize that they’re not the only person that’s experiencing that problem. There are 6,000 relatively complete case histories [on SurvivingAntidepressants]. You realize it’s all the same story. It’s one story.
And each person who experiences it is so surprised that it happened to them — people go through a period of absolute disbelief. They realize that they’ve been trusting their doctors to have a certain amount of knowledge, and their doctors don’t actually have that knowledge.
And you know, this is heartbreaking. I went through this, and I felt that the world had fallen out from underneath me. There wasn’t any medical safety net. So the sociological phenomenon exists, and has not yet filtered into medicine [this is also exactly what has happened with the COVID-19 vaccines].
Medicine has its own ways of gathering information, and in psychiatry, for some reason, they keep asking each other what the truth is instead of asking their patients. The patient voice is not very well recognized in psychiatry at all.29
Additionally, less severe (and often fluctuating) withdrawal symptoms also occur such as:
The feeling of an electric shock in your arms, legs, or head (these horrible things are commonly referred to as “brain zaps” and have happened to so many people I know)
Dizziness (mild to severe)
Visual problems
A large number of sensitivities (e.g., to light, heat, a supplement or food)
Anxiety which comes and goes, sometimes in intense ‘surges’
Difficulty in getting to sleep and vivid or frightening dreams
Low mood, feeling unable to be interested in or enjoy things
A sense of being physically unwell
Rapidly changing moods (e.g., spontaneous weeping spells, attacks of sheer terror, or sudden plunges into unprecedented contentless black holes of pure dread)
Anger, sleeplessness, tiredness, loss of co-ordination and headache
A feeling that things are not real (‘derealisation’), or a feeling that you have ‘cotton wool in your head’
Difficulty in concentrating
Suicidal thoughts
Queasiness or indigestion
A feeling of inner restlessness and inability to stay still (this is known as akathisia and often precedes psychotic SSRI violence)
Crippling muscle pain or spasms
Furthermore, these reactions are very common. A recent meta-analysis found that 56% of patients who stop using SSRIs experience withdrawals, that 46% who stop an SSRI experience severe withdrawals, and that these withdrawals last for weeks to months. Additionally, it is well known in the SSRI recovery community that the risk of a withdrawal varies greatly depending on the drug (Paxil is notorious for this, Cymbalta is also a common offender).30
Note: A 1996 door to door survey of 2003 randomly selected people in England found that 78% of them considered SSRIs to be addictive.31
Sadly, the industry is well aware of this, to the point they will often deliberately put “placebo” subjects in SSRI trials into withdrawals (by terminating their existing prescription) so they can dishonestly make the drug group look “better” than the “placebo” patients.
Pharmaceutical companies are frequently accused of operating as “organized drug dealers,” an argument especially common with SSRIs due to their (addictive) potential for dependence and how aggressively they are promoted to everyone.
Conclusion
Since the pharmaceutical industry is fundamentally driven by a need to maximize sales, drugs will routinely be brought to market that benefit a small subset of patients but then be marketed to an ever increasing number of people (e.g., the SSRI manufacturers invested heavily in convincing the public normal emotions actually “needed” lifelong SSRI treatment and that depression is a “chemical imbalance in the brain” despite no evidence supporting this).
Because of this, these mass marketed ‘blockbuster’ drugs frequently cause far more harm than any benefit they can provide. As such, members of the population are typically on multiple drugs like this (e.g., statins for “high” cholesterol), this results in healthcare costs continually going up while the general populace becomes sicker and sicker.
This downhill spiral must stop, and for the first time in my lifetime, the political will to acknowledge and address the harms overprescribed pharmaceutical drugs are inflicting upon society at last exists (e.g., consider RFK’s recent statements on antidepressants).
For things to shift, it is imperative for each of us to begin openly discussing these taboo subjects and make those we care about be aware of the real risks from pharmaceutical medications doctors rarely warn us about. I thank each of you for doing that and helping to end this; far too many people I know have had their lives ruined by SSRI antidepressants.
Author’s Note: This is an abridged version of a longer article which discusses the above points in much more detail (e.g., who benefits from SSRIs, how to safely withdraw from them) along with reviewing alternative treatment options such as psychedelic assisted psychotherapy.
That article and its additional references can be read here. Additionally, a companion article about the depression industry (e.g., how marketers managed to convince everyone they were depressed) and effective natural therapies for depression can be read here, while a companion article about the anxiety industry, natural therapies for anxiety and the dangers of benzodiazepines can be read here.
A Note from Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician from the Midwest and a longtime reader of Mercola.com. I appreciate AMD’s exceptional insight on a wide range of topics and am grateful to share it. I also respect AMD’s desire to remain anonymous since AMD is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
Disclaimer: The entire contents of this website are based upon the opinions of Dr. Mercola, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked.
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Mercola and his community. Dr. Mercola encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. The subscription fee being requested is for access to the articles and information posted on this site, and is not being paid for any individual medical advice.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.