Download Interview Transcript | Download my FREE Podcast | Video Link
STORY AT-A-GLANCE
High iron is an under-recognized health threat. There’s a general lack of awareness in the medical community regarding the potential health risks associated with high iron levels
A ferritin level above 100 typically means you're either inflamed, have high iron, or both. A level above 200 is considered pathological. The higher your ferritin level, the shorter your lifespan. You’re also more likely to die of a heart attack and cancer
Left untreated, high iron levels can cause liver damage and an increased susceptibility to certain diseases, including infections and cancer
Lab tests that can help diagnose iron-related conditions such as hemochromatosis include a full iron panel, a complete blood count (CBC) test, gamma-glutamyl transferase (GGT), and a comprehensive metabolic panel to ensure you have sufficient liver enzymes. Measuring your copper and ceruloplasmin levels can also be helpful
The easiest way to lower your iron is to donate blood on a regular basis. Natural supplements such as curcumin, silymarin, and alpha-lipoic acid can also help prevent from continuing to accumulate iron from your food
In this interview, Christy Sutton, D.C., reviews the dangers of excessive iron. While most doctors look for iron deficiency, few ever pay attention to elevated iron. Sutton is the author of two books, “Genetic Testing: Defining Your Path to a Personalized Health Plan: An Integrative Approach to Optimize Health,” and “The Iron Curse: Is Your Doctor Letting High Iron Destroy Your Health?”
Iron plays an important role in health, especially for children and young adults. Without sufficient iron, you're not going to be able to form red blood cells and certain proteins in your mitochondria that are responsible for producing energy. On the flip-side, an excess of iron can cause significant damage.
A Silent Epidemic
Sutton’s interest in iron has been “lifelong” she says, as she struggled with low iron while her husband has a genetic anomaly that causes him to have elevated iron levels. So, she has personal experience with both ends of the spectrum.
“I have Crohn's [disease], celiac, and lost part of my small intestine due to Crohn's when I was 16,” she says. “Because of that, I have to take a bile sequestrant. Then, being [a] menstruating female who's had a child, low iron has been something that I have been watched very closely for and I had to take iron a lot.
Like a lot of clinicians, when I came into practice, I seemed to be more hyper-focused on people's problems that were my own problems. I dealt with iron issues. So, I wanted to watch my patients' iron levels closely. Then I realized, ‘Oh, not everybody is low. A lot of people actually have high iron.’
It wasn't until I was writing my first book, ‘Genetic Testing: Defining Your Path to a Personalized Health Plan,’ that I discovered the hemochromatosis genes. I realized that my husband had a hemochromatosis gene, and I realized that that was why I kept telling him to donate blood.
His doctor would order iron labs, ferritin, CBC, and he would get elevated iron often, high ferritin. He was developing high liver enzymes and his red blood cells were getting high as well, which is a common issue with people that have too much iron ...
He went to a gastroenterologist, because he was trying to figure out why his liver enzymes were high. I thought it was the high iron, but that was presented to the gastroenterologist and dismissed. So, they went down this rabbit hole of misdiagnosing him with autoimmune hepatitis.
Later we went to a hematologist where we figured out he had hereditary hemochromatosis. So, it's not something that's particularly difficult to treat. Removing blood, diet supplements, things like that can help.
But once I got really savvy about looking for the genes and the labs combined, I realized that this is a silent epidemic that is not really being talked about. I would tell people, ‘You have a problem with high iron,’ and then they would often go and get a second opinion.
Their second opinion would say, ‘You're fine. Don't worry about it,’ which is a common issue where people are getting high iron labs that should warrant more investigation and then they're just getting dismissed.”
How to Lower Your Iron Level
I have beta thalassemia, a hemolytic anemia that results in a high turnover of red blood cells. My red blood cells only live about two months, rather than the normal three months. As a result, my iron tends to accumulate because of the rapid turnover. So, while I do not have the hemochromatosis gene, it results in similar problems. I inherited it from my father, who had a ferritin level close to 1,000 by the time he was diagnosed. Ideally, it should be below 40.
One of the supplements he tried was inositol, also referred to as hexaphosphate or IP-6, but it did nothing. I rapidly came to the conclusion that the supplements typically recommended for high iron are useless and in some cases even dangerous, because they prevent you from doing what is really helpful, which is to remove iron through regular phlebotomies.
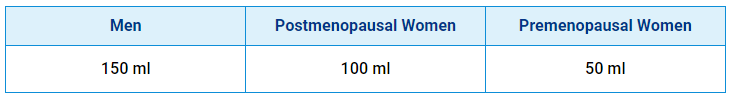
The most effective way to lower your iron is to donate blood two to four times a year. If losing 10% of your blood in one sitting is problematic for you, then you can remove blood in smaller amounts once a month on the schedule I have listed below. If you have congestive heart failure or severe COPD, you should discuss this with your doctor, but otherwise this is a fairly appropriate recommendation for most.
As it turns out, Sutton did not include IP-6 in her book, as she couldn't find any research to back up the claims. She doesn’t dismiss all supplements, however. One of the most helpful, in her view, is curcumin.
“Clinically, I have seen curcumin's ability to lower iron almost to a fault,” she says. “It's annoying to me, because I can't take curcumin for inflammation because it makes me low in iron. But for people that are high in iron or even inflamed with high iron, high ferritin, that's a great place to start, because curcumin binds to iron.
It also has all of these other wonderful health promoting properties. It's so good for your brain — it actually helps remove excess iron from the brain and other organs, the heart, liver, spleen.
So, unlike other iron chelators that might be used pharmaceutically, it doesn't have all these possible negative side effects, but it works very effectively. I mean, I've seen it be used in hereditary hemochromatosis patients to lower iron without blood removal ... Now, people that have really high iron might need 3 grams a day, which can create diarrhea. So, you have to look at other potentially limiting factors.”
She also recommends taking curcumin with an iron-rich meal, such as shellfish or red meat, to inhibit iron uptake. Other supplements that help bind iron include silymarin, (an extract from milk thistle). It too is very good for hemochromatosis patients, because it lowers iron and helps protect and repair the liver. Another thing that binds to and lowers iron is alpha-lipoic acid. It’s also great for protecting nerves and lowering blood sugar.
“I don't think silymarin lowers iron quite as much as curcumin, but it's still a significant way to lower iron,” she says. “The best way to take these — to lower iron — is take them with iron-rich meals. If you want to take them just for medicinal properties but not to lower iron, take them away from iron-rich meals.”
Health Risks Associated with High Iron
The health risks of high iron are manifold and include an elevated risk of skin infections and skin cancer. I suspect high iron may actually be a catalyst when it comes to skin cancer, along with high linoleic acid (LA) intake. LA is oxidized by iron, creating something called lipofuscin, which is basically iron attached to oxidized LA.
A more common term for lipofuscin is liver spots. So, liver spots are a dermal representation of oxidative damage to LA by high iron. Similarly, skin cancer is likely driven by a combination of high LA and high iron. Ancestral LA levels were below 2%. Today, the average is around 25%. If you had normal ancestral levels, you could have higher iron yet not get as much damage.
Understanding Hemochromatosis
There are several potential diagnoses related to iron, including iron-deficient anemia, copper deficient anemia, iron overload and hereditary hemochromatosis, and getting to the correct diagnosis can be tricky.
“The nice thing is that you can always fall back on labs,” Sutton says. “You don’t want to just use symptoms to guide you, because if you’re using symptoms, then this person is well far down a pathological path that you could have potentially stopped years ago, if not decades before.”
Starting with hereditary hemochromatosis, this is when you have inherited one of three hemochromatosis genes, which causes increased iron absorption by decreasing hepcidin, a liver protein. If you have the hemochromatosis gene, you don’t make as much hepcidin, causing you to absorb more iron.
That can become pathological, because over time, you just keep absorbing more and more iron, until your body finally runs out of places to put it. The first place that gets overloaded is your liver. After that, your body will store the iron in other organs, such as your heart, pancreas, brain, pituitary gland, gonads, ovaries, testes, and skin.
Eventually, the iron will go everywhere because the human body has evolved to hold onto as much iron as possible. The only way, really, to lose iron is through blood loss. This is why menstruating women have a lower risk for high iron and a higher risk for low iron.
“Having said that, when you start looking at the hemochromatosis genes, all bets are off, because you’ll see females that have these hemochromatosis genes that develop high iron … you will even see children with the hemochromatosis genes that develop high iron,” Sutton says.
“I discovered that in my colleague’s 5-year-old, where predatory hemochromatosis was causing her to have severe neurological problems. That was a very difficult thing to get through because the hematologist didn’t really want to deal with it.
When you look at labs, hereditary hemochromatosis can look very similar to non-hereditary hemochromatosis, which is where you have high iron but you don’t have one of those hemochromatosis genes.
So, for you, you have more of a non-hereditary secondary hemochromatosis, because you have that thalassemia issue where your red blood cells are breaking and letting all this iron out and then you develop high iron with potentially low red blood cells.
That's common with thalassemia. Some people, they don’t have a thalassemia gene and they develop high iron without hemochromatosis gene, because they’re just eating a lot of iron-rich foods and they’re not losing iron through menstruation. This is usually men.”
How to Diagnose Hemochromatosis
When it comes to lab work, Sutton recommends starting with a full iron panel, a complete blood count (CBC) test, gamma-glutamyl transferase (GGT), and a comprehensive metabolic panel to ensure you have sufficient liver enzymes. Measuring your copper and ceruloplasmin levels can also be helpful.
“The full iron panel has the ferritin, the TIBC [total iron-binding capacity], the UIBC [unsaturated iron-binding capacity], the serum iron and the iron saturation. With hereditary hemochromatosis, you develop high ferritin with a high iron saturation. That combination is hereditary hemochromatosis. So, over 45% iron saturation and high ferritin ...
With hereditary hemochromatosis, you’ll see high iron, you’ll see the TIBC go low, the UIBC go low. The serum iron often goes high, and then that ferritin will go high. You’ll often see the liver enzymes go high and it's common to see the red blood cells, hemoglobin, hematocrit go high.
But that doesn’t always happen. These days, so many are taking testosterone. So, you have to always ask, ‘Are you on testosterone?’ Because that can cause red blood cells, hemoglobin, hematocrit to go high as well ...
I always get the GGT as a part of the labs that I order. Occasionally, I will see a high GGT when the AST and ALT, which are the other two liver enzymes, are normal. More often than not, I’ll see a high ALT or high AST. Usually, if they’re not drinking alcohol and they just have high iron, you’re going to see that high ALT.”
What’s the Ideal Ferritin Level?
Sutton recommends keeping ferritin below 100. Ferritin above 100 means you’re either inflamed, have high iron or both. Studies referenced in her book suggest that anything over 200 is pathological. The higher your ferritin level, the shorter your lifespan. You’re also more likely to die of a heart attack and cancer.
“I feel like 100 is high enough that I’m not swooping everybody in, but low enough that I’m not leaving stragglers out,” she says. “Now, if somebody has a ferritin over 100 with an iron saturation that is in the 40s or higher, then I’m highly suspicious of a hemochromatosis gene and I immediately want to get those hemochromatosis genes tested.
If they have a hemochromatosis gene, then we know why they’re high on iron and we know where this story is going — and it’s not going to be a pretty picture most likely. Then it’s time to refer to a hematologist ... and talk to them about how to get iron lower ...
The key is, if you don’t have a hemochromatosis gene, then you need to figure out ‘Why does this person have high iron? Do they have a thalassemia gene? Are they just eating a lot of iron?’ And then, ‘Do they have hemolysis for some unknown reason?’ That’s a non-hereditary hemochromatosis situation.
The treatment is basically the same, other than you want to use more of the supplements, go really heavy on the supplements to lower iron. If you have plenty of red blood cells and hemoglobin, then therapeutic phlebotomy is a wonderful place to start.
A lot of times people don’t because they either have a thalassemia issue where their red blood cells are getting chewed up too quickly, or they have lost so much blood so quickly because their doctors are just trying to get the iron down that they become low in hemoglobin or red blood cells. Rather than waiting for months for that to recover, you could be doing the supplements to lower the iron.”
The Link Between High Iron and Cushing’s Disease
Sutton’s husband also developed a pituitary tumor that was causing him to have high cortisol (Cushing’s disease). “Ultimately, I think the high iron created a lot of oxidative stress on his pituitary gland,” Sutton says. The only reason he was diagnosed early enough to save him was that they’d been checking his cortisol and DHEA on a regular basis.
“Periodically, they would jump up and then go back down. Then when the hemochromatosis got properly treated and the DHEA was still high, we were like, ‘Why is this happening?’ So we went to the endocrinologist and I said, ‘I’m worried my husband has Cushing’s.’ She was like, ‘He doesn’t have Cushing’s. He doesn’t look like somebody with Cushing’s. His hemoglobin A1C is normal.’
Five months later, he’s having surgery to remove the pituitary tumor. The reason I say that is because for years, he was told, ‘You just need to exercise and lose weight.’ His problem was not exercise. He had a pituitary tumor and hemochromatosis. Hemochromatosis was destroying his liver and his brain and his heart and everything else, and the pituitary tumor was causing him to have high cortisol, which made him look overweight.”
I believe progesterone may be one of the best ways to treat Cushing’s disease, as it very effectively blocks cortisol. Other natural substances that will inhibit cortisol include aspirin, DHEA, pregnenolone, emodin, vitamins A and D, gelatin or glycine, and niacinamide.1
The normal dose for progesterone is 25 to 50 milligrams. For Cushing’s, I would recommend about 300 mg. It’s virtually impossible to overdose on progesterone and there are no downsides to it. One caveat is that you need to administer it correctly to gain the optimal effects.
How to Use Progesterone
Before you consider using progesterone, it is important to understand that it is not a magic bullet, and that you get the most benefit by implementing a Bioenergetic diet approach that allows you to effectively burn glucose as your primary fuel without backing up electrons in your mitochondria that reduces your energy production. My new book, "Your Guide to Cellular Health: Unlocking the Science of Longevity and Joy," covers this process in great detail.
Once you have dialed in your diet, an effective strategy that can help counteract estrogen excess is to take transmucosal progesterone (i.e., applied to your gums, not oral or transdermal), which is a natural estrogen antagonist. Progesterone is one of only three hormones I believe many adults can benefit from. (The other two are DHEA and pregnenolone.)
I do not recommend transdermal progesterone, as your skin expresses high levels of 5-alpha reductase enzyme, which causes a significant portion of the progesterone you're taking to be irreversibly converted primarily into allopregnanolone and cannot be converted back into progesterone.
Ideal Way to Administer Progesterone
Please note that when progesterone is used transmucosally on your gums as I advise, the FDA believes that somehow converts it into a drug and prohibits any company from advising that on its label. This is why companies promote their progesterone products as "topical."
However, please understand that it is perfectly legal for any physician to recommend an off-label indication for a drug to their patient. In this case, progesterone is a natural hormone and not a drug and is very safe even in high doses. This is unlike synthetic progesterone called progestins that are used by drug companies, but frequently, and incorrectly, referred.
Dr. Ray Peat has done the seminal work in progesterone and probably was the world's greatest expert on progesterone. He wrote his Ph.D. on estrogen in 1982 and spent most of his professional career documenting the need to counteract the dangers of excess estrogen with low-LA diets and transmucosal progesterone supplementation.
He determined that most solvents do not dissolve progesterone well and discovered that vitamin E is the best solvent to optimally provide progesterone in your tissue. Vitamin E also protects you against damage from LA. You just need to be very careful about which vitamin E you use as most supplemental vitamin E on the market is worse than worthless and will cause you harm not benefit.
It is imperative to avoid using any synthetic vitamin E (alpha tocopherol acetate — the acetate indicates that it's synthetic). Natural vitamin E will be labeled "d alpha tocopherol." This is the pure D isomer, which is what your body can use.
There are also other vitamin E isomers, and you want the complete spectrum of tocopherols and tocotrienols, specifically the beta, gamma, and delta types, in the effective D isomer. As an example of an ideal vitamin E, you can look at the label on our vitamin E in our store. You can use any brand that has a similar label.
You can purchase pharmaceutical grade bioidentical progesterone as Progesterone Powder, Bioidentical Micronized Powder, 10 grams for about $40 on many online stores like Amazon. That is nearly a year's supply, depending on the dose you choose.
However, you will need to purchase some small stainless steel measuring spoons as you will need a 1/64 tsp, which is 25 mg and a 1/32 tsp, which is 50 mg. A normal dose is typically 25 to 50 mg and is taken 30 to 60 minutes before bed, as it has an anti-cortisol function and will increase GABA levels for a good night's sleep.
If you are a menstruating woman, you should take the progesterone during the luteal phase or the last half of your cycle, which can be determined by starting 10 days after the first day of your period and stopping the progesterone when your period starts.
If you are a male or non-menstruating woman, you can take the progesterone every day for four to six months and then cycle off for one week. The best time of day to take progesterone is 30 to 60 minutes before bed as it has an anti-cortisol function and will increase GABA levels for a good night's sleep.
This is what I have been personally doing for over a year with very good results. I am a physician so do not have any problems doing this. If you aren't a physician, you should consult one before using this therapy, as transmucosal progesterone therapy requires a doctor's prescription.
Understanding Iron-Deficient Anemia
As explained by Sutton, iron-deficient anemia is a serious issue. Children born of women with iron-deficient anemia have significantly higher risk of low IQ, ADD, ADHD, and other neurological issues that often do not go away with age.
“Many kids suffer from low iron, because they eat a lot of calcium rich foods. Calcium binds to iron, and then you get low in the iron. Maybe they’re picky eaters, they’re growing rapidly. So many kids are not being checked for their iron levels and they’re being diagnosed with ADHD when their problem is actually just low iron, because if you don’t have enough iron, you can’t make dopamine. So, low iron is a serious issue.”
People with iron-deficient anemia will typically have high TIBC and UIBC, as their bodies are trying to mobilize more iron. Serum iron and iron saturation will be low and ferritin will typically be below 30.
“Now, iron-deficient anemia is more complicated in many ways because the question is, why are you low in iron?” Sutton says. “There’s so many reasons that you can be low in iron. Are you just not eating enough? Are you not absorbing it? I think the most common reasons that people develop low iron is because they have a GI bleed. They have intestinal malabsorption issues, maybe undiagnosed celiac disease.
There is a gene that can cause you to be more likely to have low iron. I have that gene and that gene actually causes you to make more hepcidin. With iron-deficient anemia you'll also see low red blood cells sometimes, low hemoglobin, and low hematocrit. MCH [mean corpuscular hemoglobin] might get low, MCV [mean corpuscular volume] might get low.”
Copper Deficiency Can Cause Both Low and High Iron
One common cause for iron-deficient anemia is a deficiency in copper. Paradoxically, lack of copper is also a common cause for iron overload. Sutton explains:
“The reason for that is because copper is necessary for two key enzymes. The first one is called hephaestin and the second one is called ceruloplasmin. Hephaestin is in the lining of the gut, the intestinal lining. Copper is necessary for iron to be absorbed in the gut lining. So, without copper, you will not absorb iron and you will develop iron-deficient anemia.
Once iron has been absorbed in the gut lining by hephaestin, it passes it off to ceruloplasmin, which is the second copper-rich enzyme. Ceruloplasmin basically then allows that copper to transfer in and then move throughout the body. So, without ceruloplasmin, iron gets stuck in the tissues. It'll get stuck in the digestive system, it'll get stuck in the retina, it'll get stuck in the brain, it'll get stuck in the liver.
So, you develop iron overload in the tissues. But eventually, if you're low in copper long enough, you might then become low in iron, and then you don't end up with all this extra iron in the tissues. The solution is take copper to fix that problem. That's the way you solve copper-deficient anemia.
Copper-deficient anemia looks very similar to iron-deficient anemia if you're looking at the iron panel. You'll have a high TIBC, high UIBC, low serum iron, low iron saturation, low ferritin. You'll also potentially see low neutrophils and low white blood cells, because you need copper to have normal immune function as well. So, you might be more at risk for infections.
Then of course you can look at the ceruloplasmin. I don't find ceruloplasmin to be the easiest lab to look at, because it's an inflammatory marker ... If you're taking hormones like estrogen or birth control or you're pregnant or you're just inflamed or have an infection, ceruloplasmin can jump around and go high.
If you have a low or low-normal ceruloplasmin, and then you take copper and ceruloplasmin goes up, that's a good sign that you didn't have enough copper.”
How to Get More Iron Into Your Diet
The best way to get iron is through your diet. Shellfish and beef are iron-rich foods with highly absorbable iron. That’s key, because there are two types of iron — heme iron and non-heme iron, the latter of which is not very absorbable. Heme iron is found in animal products while non-heme iron is found in vegetables such as spinach.
“If you're not eating iron-rich foods like red meat, then you're more likely to get low in iron if that is something that you struggle with,” Sutton says. “If you struggle with being high in iron, maybe you don't want to eat as many of those things or maybe you just want to remove blood and supplement accordingly, so that you continue to eat those things.
The form that I like if I'm going to go to a supplement is ferrous peptonate, which I found to be the gentlest on my gut but also get the iron levels up. I really don't like ferrous sulfate, which is the most common given iron. I don't think it works very well, and it tends to create a lot of stomach pain. I always have to take my iron with food and sometimes I'll add copper or vitamin C to it. If I don't take it with food, it's really going to upset my stomach.”
More Information
To learn more, check out Sutton’s books, “Genetic Testing: Defining Your Path to a Personalized Health Plan: An Integrative Approach to Optimize Health,” and “The Iron Curse, Is Your Doctor Letting High Iron Destroy Your Health?”
Disclaimer: The entire contents of this website are based upon the opinions of Dr. Mercola, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked.
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Mercola and his community. Dr. Mercola encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. The subscription fee being requested is for access to the articles and information posted on this site, and is not being paid for any individual medical advice.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your health care professional before using products based on this content.